AIDS Risk Assessment Tool
Condoms: Highly effective when used correctly during every sexual act.
PrEP: Daily medication for HIV-negative individuals at high risk; up to 99% effective.
Treatment as Prevention (TasP): Effective for HIV-positive individuals with suppressed viral load.
PEP: Emergency medication started within 72 hours after potential exposure.
Ever wondered why AIDS still makes headlines despite all the medical advances? You’re not alone. This guide breaks down the disease in plain language, shows you what to look out for, and gives you the tools to protect yourself and others.
What is AIDS?
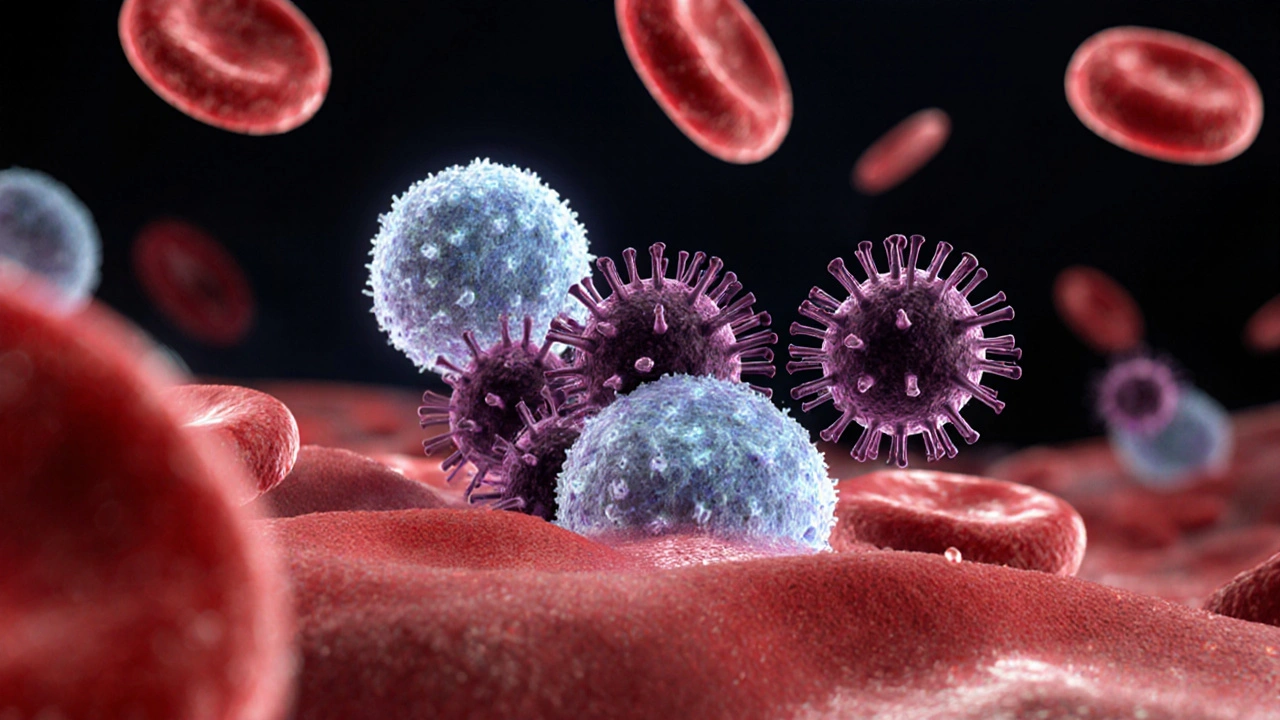
AIDS is the final stage of HIV infection, where the immune system is severely damaged and the body becomes vulnerable to opportunistic infections and cancers. In everyday terms, think of your immune system as a security guard. When HIV (Human Immunodeficiency Virus) infiltrates, it weakens that guard over years, and once the guard can’t do its job, AIDS appears.
How HIV Leads to AIDS
HIV is a retrovirus that targets CD4+ T‑cells, the white blood cells that coordinate the immune response. By attaching to these cells, HIV hijacks them to make copies of itself, gradually destroying them. The immune system a network of cells, tissues, and organs that defends against disease relies on CD4+ cells, so when their count drops below 200 cells per microliter, the body can’t fight off everyday germs - that’s when doctors diagnose AIDS.
Key Causes & Transmission Routes
- Unprotected vaginal, anal, or oral sex with an infected partner.
- Sharing needles or syringes for drugs, tattoos, or piercings.
- Mother‑to‑child transmission during pregnancy, birth, or breastfeeding.
- Rarely, through blood transfusions that haven’t been screened.
It’s worth noting that HIV does NOT spread through casual contact - no hugging, sharing dishes, or using the same toilet.
Symptoms: From Early Signs to Advanced AIDS
HIV can be sneaky. Early after infection, many people feel fine. When symptoms do show up, they often mimic flu‑like illness:
- Fever, night sweats, and chills.
- Swollen lymph nodes (especially in the neck and groin).
- Weight loss and loss of appetite.
- Persistent fatigue.
As the virus progresses and CD4 counts fall, more serious signs appear, such as:
- Severe or recurring infections (pneumonia, tuberculosis, thrush).
- Unexplained skin rashes or lesions.
- Neurological problems - memory loss, confusion, or peripheral neuropathy.
- Certain cancers like Kaposi’s sarcoma or non‑Hodgkin lymphoma.
If you notice a cluster of these symptoms, especially after a possible exposure, get tested right away.
Getting Tested: Know Your Status
HIV test a quick blood or oral fluid test that looks for antibodies, antigens, or viral RNA is the only way to confirm infection. In many places you can:
- Visit a community health clinic for a free rapid test (results in 20 minutes).
- Order a home‑collection kit online and mail it to a lab.
- Ask your GP for a standard laboratory test (more accurate for early infection).
Most tests are confidential, and if the result is positive, you’ll receive counseling on next steps - treatment, partner notification, and support services.
Prevention: How to Stay Safe
There’s no single magic bullet, but combining methods gives the highest protection. Below is a quick comparison of the most common strategies.
| Method | Effectiveness (when used correctly) | How It Works | Frequency / Duration | Typical Cost (AU$) |
|---|---|---|---|---|
| Condom latex or polyurethane barrier used during sex | ≈ 80‑95% | Physically blocks virus from entering bodily fluids | Every act of vaginal, anal, or oral sex | 0.5‑2 per piece |
| Pre‑exposure prophylaxis (PrEP) daily oral medication (e.g., tenofovir/emtricitabine) that prevents HIV infection | ≈ 99% when taken daily | Maintains drug level in blood that stops virus from establishing infection | One pill daily | 30‑50 per month (subsidised in many Australian states) |
| Treatment as Prevention (TasP) antiretroviral therapy that suppresses viral load in HIV‑positive people | ≈ 0% transmission risk when viral load < 200 copies/mL | Reduces amount of virus in blood, making it virtually untransmittable | Daily medication regimen | Covered by Medicare for eligible patients |
Other useful steps include regular testing, limiting the number of sexual partners, and avoiding sharing needles. If you’re already living with HIV, staying on antiretroviral therapy a combination of medicines that suppress HIV replication not only protects your health but also prevents you from passing the virus to others.

Living with AIDS: Care and Support
Being diagnosed with AIDS can feel overwhelming, but modern medicine has turned it from a death sentence into a manageable chronic condition. Key steps include:
- Adhering to your antiretroviral therapy schedule - missing doses can let the virus rebound.
- Regular monitoring of CD4 count a lab measurement of immune health and viral load.
- Vaccinations against flu, pneumococcus, and hepatitis B to prevent opportunistic infections.
- Connecting with local support groups - many Australian cities run free counselling and peer‑support programs.
Nutrition, exercise, and mental health care also play a big role. A balanced diet rich in protein, fruits, and vegetables helps maintain immune strength, while stress‑relief activities can boost overall wellbeing.
Quick Checklist: What to Do If You Suspect Exposure
- Stop any ongoing risk activity (e.g., use a condom, discard a used needle).
- Find a testing site - many pharmacies offer rapid tests without an appointment.
- If the test is positive, schedule a follow‑up with a specialist for baseline labs (CD4, viral load).
- Discuss starting antiretroviral therapy ASAP - early treatment improves outcomes.
- Inform recent partners so they can get tested and, if needed, start post‑exposure prophylaxis (PEP) within 72 hours.
Remember, early action saves lives and reduces the chance of onward transmission.
Frequently Asked Questions
Can AIDS be cured?
There is currently no cure for HIV or AIDS, but antiretroviral therapy can suppress the virus to undetectable levels, allowing people to live long, healthy lives.
How long does it take for HIV to progress to AIDS?
Without treatment, the average time from HIV infection to AIDS is about 8‑10 years, but it can be faster or slower depending on health, age, and other factors.
Is it safe to have oral sex with an HIV‑positive partner?
The risk of HIV transmission through oral sex is very low, especially if there are no open sores or bleeding gums. Using a barrier (condom or dental dam) further reduces any risk.
What is the difference between PrEP and PEP?
PrEP (pre‑exposure prophylaxis) is taken daily by HIV‑negative people to prevent infection before exposure. PEP (post‑exposure prophylaxis) is a short‑term (28‑day) medication started within 72 hours after a possible exposure.
Can I get HIV from a tattoo?
Only if the tattoo equipment is contaminated with infected blood. Licensed studios must use sterile, single‑use needles, making the risk negligible.

Comments
Sidney Wachira
Wow, this guide is a lifesaver! 😊
October 6, 2025 at 12:19
Aditya Satria
Great job breaking down HIV transmission routes so clearly. The step‑by‑step risk assessment makes it easy for anyone to understand their personal risk. I also appreciate the inclusion of both PrEP and PEP options, which often get overlooked. Keep sharing such thorough resources.
October 12, 2025 at 03:02
Jocelyn Hansen
Absolutely love how this guide walks you through every stage-from basic definitions to actionable prevention! 🌟 The tables and checklists are super handy, especially the quick‑reference chart on condom effectiveness. It’s also reassuring to see the emphasis on regular testing and early treatment. Readers will feel empowered to take control of their health after reading this! Keep up the fantastic work!!
October 17, 2025 at 17:45
Joanne Myers
The information presented is comprehensive and well‑structured, offering clear guidance on both prevention and management of HIV/AIDS.
October 23, 2025 at 08:29
rahul s
Finally, a piece that doesn’t sugarcoat the reality of HIV-this stuff is straight‑up crucial for anyone who cares about staying safe in today’s world. The stats and prevention tactics are laid out with no nonsense, and anyone ignoring this is just asking for trouble.
October 28, 2025 at 22:12
Tommy Mains
Thanks for the compliment! If you’re looking for a quick way to start testing, many pharmacies now offer rapid tests that give results in under half an hour. Just grab a kit, follow the instructions, and you’ll have peace of mind fast. Stay safe out there.
November 3, 2025 at 12:55
Oscar Brown
The depth of this guide is impressive, offering a solid foundation for newcomers and seasoned advocates alike.
Each section builds logically, beginning with the virology of HIV and culminating in actionable public‑health strategies.
The inclusion of quantitative data, such as the 99% efficacy figure for PrEP, enhances credibility.
Furthermore, the risk‑assessment tool serves as a practical bridge between theory and personal decision‑making.
By outlining both biomedical and behavioral interventions, the article respects the multifaceted nature of disease prevention.
The discussion of viral latency and reservoir formation is particularly valuable for understanding why early treatment matters.
It also clarifies why adherence to antiretroviral therapy is non‑negotiable.
Readers are reminded that even with suppressed viral loads, ongoing monitoring remains essential.
The emphasis on stigma reduction and community support underscores the social dimension of health.
In addition, the clear tabular comparisons make complex data accessible.
These tables help demystify the differences between condoms, PrEP, TasP, and PEP.
Such visual aids are indispensable for educators and patients alike.
The article’s tone balances urgency with hope, motivating proactive health behavior.
Overall, the piece exemplifies how comprehensive health communication should be crafted.
It stands as a model for future public‑health publications.
November 9, 2025 at 03:39
Amanda Mooney
Your appreciation is noted, and indeed the structured layout aids comprehension. Moreover, the inclusion of both medical and lifestyle advice creates a holistic approach.
November 14, 2025 at 18:22
Alex Feseto
The articulation of epidemiological data herein is commendably rigorous, offering a discerning reader an edifying perspective on viral pathogenesis.
November 20, 2025 at 09:05
Julie Sook-Man Chan
Noted. The pharmacy route is indeed convenient for many.
November 25, 2025 at 23:49
vedant menghare
The nuance you’ve captured regarding viral latency and reservoir dynamics is particularly insightful. It underscores why adherence to antiretroviral therapy is non‑negotiable. Additionally, the societal stigma component you mentioned cannot be overstated; education remains the linchpin.
December 1, 2025 at 14:32
Natasha Beynon
Glad you find the approach holistic! It truly bridges the gap between clinical guidelines and everyday choices.
December 7, 2025 at 05:15
Cinder Rothschild
Indeed, the precision of the data presentation elevates the discourse surrounding HIV prevention. When the statistics are laid out with such clarity, it compels policymakers to allocate resources more judiciously. Furthermore, the visual aids-like the comparative table-serve as an invaluable tool for educators. By demystifying the efficacy percentages, we empower individuals to make informed decisions. The guide also rightly points out that behavioral interventions complement biomedical strategies. In sum, this synthesis of information is exactly what the public health community needs to disseminate widely.
December 12, 2025 at 19:59
Robyn Chowdhury
Whoa, the thread is getting deep! 😱 It’s amazing how a simple comment can spiral into a full‑blown discussion about public health.
December 18, 2025 at 10:42
Kevin Cahuana
Reading this article reminded me how crucial community support is for those living with HIV. It’s not just about meds; the emotional backing from friends and support groups makes a massive difference. If anyone’s feeling isolated, reaching out to local groups can provide that needed connection.
December 24, 2025 at 01:25
Deb Kovach
Absolutely, the psychosocial aspect is often under‑emphasized. Engaging with peer networks can improve adherence to treatment and overall wellbeing. 😊
December 29, 2025 at 16:09
Danielle Ryan
Sure, but remember the pharma giants have their own agenda-don’t let them pull the strings! They profit off our fears, so stay vigilant!!!
January 4, 2026 at 06:52
Mandie Scrivens
Interesting how a single article can pack so many facts and still manage to be readable.
January 9, 2026 at 21:35
Write a comment