Albuterol Food Checker
Check Food Safety for Albuterol Users
Enter a food or select from the list below to see if it's recommended when using albuterol for asthma.
When you rely on Albuterol is a short-acting beta‑agonist bronchodilator used to relieve asthma symptoms, what you eat can change how well it works. Asthma is a chronic inflammatory airway disease that causes wheezing, shortness of breath and coughing doesn’t just respond to medication - diet can amplify or blunt the relief you get from each puff.
Quick Takeaways
- High‑sulfite and high‑histamine foods can trigger bronchospasm and make albuterol diet challenges worse.
- Acidic, dairy‑heavy, and heavily processed meals may increase throat irritation and reduce bronchodilator effectiveness.
- Omega‑3 rich fish, vitamin‑D fortified foods, and antioxidant‑packed fruits support airway calmness.
- Stay hydrated, space meals 1‑2 hours away from inhaler use, and keep a simple food‑symptom log.
- Combine dietary changes with regular medical review for the best long‑term asthma control.
Why Diet Matters When You Use Albuterol
Albuterol works by relaxing the smooth muscle around your airways. However, certain foods can provoke inflammation or cause the airways to become extra sensitive, demanding more frequent puffs. In addition, some nutrients affect the metabolism of beta‑agonists, either speeding up clearance (making the dose wear off faster) or slowing it down (increasing tremor or heart‑racing side effects).
Foods to Avoid
Most of the “no‑go” items share a common theme: they either release histamine, contain sulfites, or are highly acidic. Both histamine and sulfite can trigger bronchial irritation, while acidity can aggravate reflux, a hidden asthma trigger.
High‑Sulfite Foods
Sulfite is a preservative that can provoke bronchospasm in sulfite‑sensitive individuals. Common culprits include:
- Wine and champagne
- Packaged dried fruits (especially apricots and raisins)
- Commercial sauces, pickles, and salad dressings
- Some processed snack foods
High‑Histamine Foods
Histamine can act like a tiny alarm that nudges your airways to tighten. Foods that are naturally high in histamine or that cause your body to release more include:
- Aged cheeses (e.g., cheddar, parmesan)
- Smoked or cured meats (salami, pepperoni)
- Fermented products (kimchi, sauerkraut, soy sauce)
- Certain fish like mackerel, tuna, and sardines when not super‑fresh
Acidic and Citrus Foods
Acidity can worsen gastro‑esophageal reflux, a known asthma aggravator. While citrus provides vitamin C, too much can backfire for some:
- Oranges, grapefruits, lemons, and limes in large quantities
- Tomato‑based sauces and ketchup
- Vinegar‑rich dressings
Dairy Products
Full‑fat milk, ice cream, and creamy sauces can increase mucus production for a subset of asthmatics, making the airway feel clogged and prompting extra albuterol use.
Highly Processed Foods
These often contain hidden sulfites, excessive sodium, and unhealthy fats that amplify systemic inflammation:
- Fast‑food burgers and fries
- Pre‑made frozen meals
- Snack chips loaded with artificial flavorings

Foods That Can Help Manage Asthma
On the flip side, some nutrients have proven anti‑inflammatory or bronchodilatory properties. Including them regularly can reduce the number of rescue inhalations you need.
Omega‑3 Fatty Acids
Omega‑3 fatty acid is a polyunsaturated fat known for reducing airway inflammation. Great sources are:
- Salmon, mackerel, sardines (prefer wild‑caught)
- Chia seeds, flaxseeds, and walnuts
Vitamin D
Vitamin D is a fat‑soluble vitamin that supports immune regulation and may lower asthma attacks. Aim for:
- Fortified dairy or plant milks
- Egg yolks
- Safe sun exposure (10‑15 minutes a few times a week)
Antioxidant‑Rich Fruits and Vegetables
Colorful produce packs vitamins C, E, and β‑carotene, which neutralize oxidative stress in lung tissue.
- Berries (blueberries, strawberries)
- Leafy greens (spinach, kale)
- Sweet potatoes and carrots
Magnesium‑Rich Foods
Magnesium relaxes smooth muscle, including bronchial tubes. Incorporate:
- Bananas
- Pumpkin seeds
- Black beans
Ginger and Turmeric
Both have natural anti‑inflammatory compounds (gingerols and curcumin) that can ease airway swelling.
- Add fresh ginger to stir‑fries or tea
- Use turmeric in soups or golden‑milk drinks
Practical Meal‑Planning Tips for Albuterol Users
- Space your inhaler use. Wait at least 30 minutes after a heavy meal before taking a rescue puff. This reduces the chance that food‑induced reflux will counteract bronchodilation.
- Hydrate well. Water helps thin mucus and supports overall lung function. Aim for 6‑8 glasses daily.
- Keep a food‑symptom log. Write down what you eat, when you take albuterol, and any changes in wheeze or coughing. Patterns emerge quickly.
- Batch‑cook anti‑inflammatory meals. A big pot of salmon‑and‑vegetable bake or a lentil‑turmeric stew can be portioned for the week, ensuring you always have a safe option on hand.
- Limit caffeine around inhaler time. Caffeine can increase heart rate, mimicking albuterol’s side effects (tremor, palpitations) and making it hard to tell what’s medication‑related.
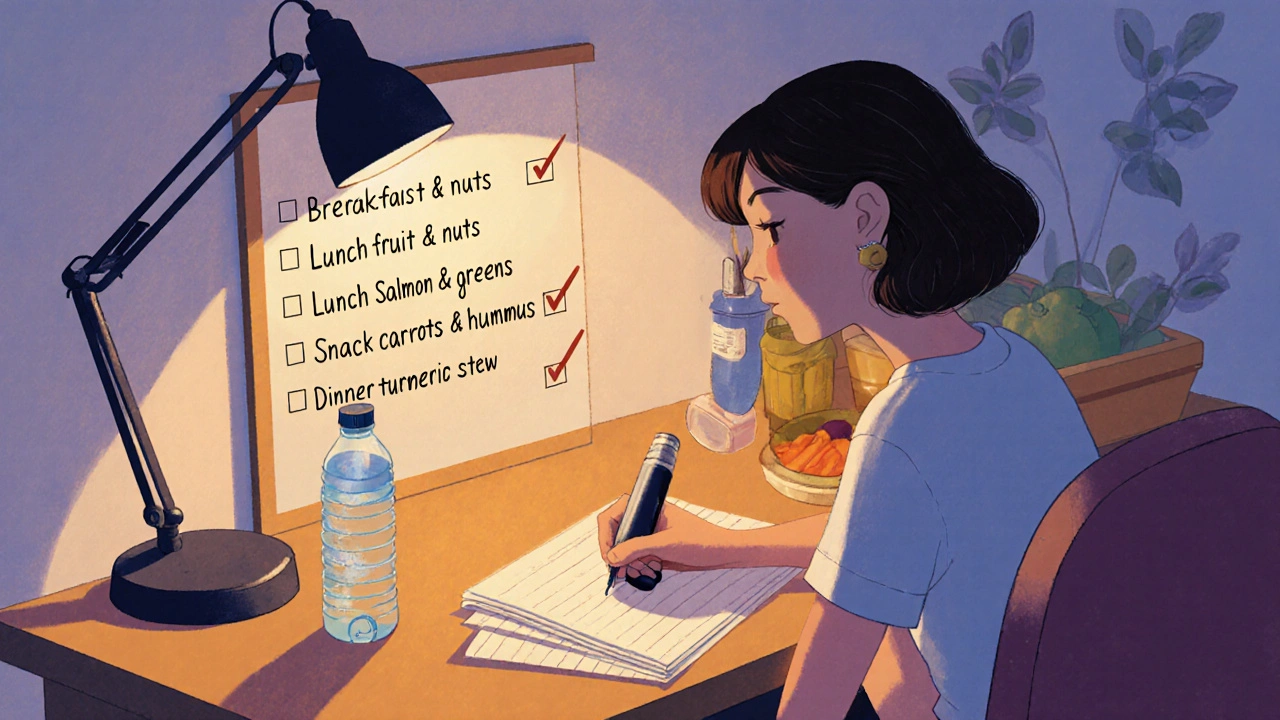
Checklist: Daily Asthma‑Friendly Eating
- ✅ Breakfast includes a fruit high in vitamin C and a handful of nuts for omega‑3.
- ✅ Lunch features leafy greens, grilled salmon, and a drizzle of olive oil.
- ✅ Snack: carrot sticks with hummus (magnesium + protein).
- ✅ Dinner: turmeric‑spiced sweet potato stew with black beans.
- ✅ No wine, dried fruit, or aged cheese after 6 PM.
Frequently Asked Questions
Can I eat citrus if I use albuterol?
Citrus provides vitamin C, which is good for the immune system, but large amounts can increase stomach acidity and trigger reflux‑related asthma symptoms. If you notice more wheezing after citrus, try smaller portions or choose low‑acid fruits like berries.
Do dairy products make albuterol less effective?
Dairy isn’t a direct antagonist to albuterol, but for some people it thickens mucus, which can make breathing feel tighter and lead to extra inhaler use. If you’re sensitive, opt for lactose‑free or plant‑based milks.
Is there a link between vitamin D levels and asthma attacks?
Research published in the Journal of Allergy and Clinical Immunology (2023) found that adults with sufficient vitamin D had 30 % fewer severe asthma exacerbations. A daily 800-1000 IU supplement is often recommended, but talk to your doctor about the right dose.
Should I avoid alcohol entirely while taking albuterol?
Alcohol itself doesn’t cancel albuterol, but wine and other sulfite‑rich drinks can provoke bronchospasm in sensitive individuals. If you enjoy a glass, choose a low‑sulfite option and observe any change in breathing.
How often should I review my diet with my asthma doctor?
A dietary check‑in every 6‑12 months works for most patients. Bring your food‑symptom log so the clinician can spot triggers and adjust medication if needed.
Bottom Line
Pairing a smart albuterol diet with your rescue inhaler can shave off extra puffs, calm inflammation, and improve overall quality of life. Focus on cutting sulfites, histamine, and acidity while loading up on omega‑3s, vitamin D, and antioxidant‑rich produce. Keep a simple log, stay hydrated, and revisit your plan with a healthcare professional regularly.


Comments
Harry Bhullar
First, it's essential to understand that albuterol's pharmacodynamics can be subtly altered by what you put on your plate.
Foods high in sulfites, like many commercial sauces and dried fruits, can provoke bronchospasm in susceptible individuals, effectively raising the threshold for a rescue inhaler to work.
Likewise, histamine‑rich items such as aged cheeses and fermented soy products may sensitize airway smooth muscle, leading to more frequent puffing.
Acidic foods, especially citrus and tomato‑based sauces, increase gastric reflux which in turn can irritate the lower airway and counteract bronchodilation.
On the flip side, omega‑3 fatty acids found in wild‑caught salmon, mackerel, and plant sources like chia seeds have been shown to dampen airway inflammation through the production of resolvins.
Vitamin D, whether obtained from fortified milks, egg yolks, or sensible sun exposure, supports immune regulation and has been correlated with a reduction in severe asthma exacerbations.
Antioxidant‑rich fruits such as blueberries, strawberries, and kale deliver vitamins C and E, which scavenge reactive oxygen species that otherwise damage epithelial cells.
Magnesium, abundant in bananas, pumpkin seeds, and black beans, relaxes smooth muscle and can modestly improve bronchodilator response.
Practical meal planning should include a 30‑minute window between a heavy meal and albuterol use, giving the stomach time to empty and reducing reflux risk.
Hydration is also key; six to eight glasses of water daily keep mucus thin and less likely to obstruct the airway.
Keeping a simple food‑symptom log allows you to spot patterns-perhaps a particular brand of dressing or a weekend brunch habit-that you might otherwise miss.
Batch‑cooking anti‑inflammatory soups or stews ensures you have a safe option on hand when cravings hit.
Limiting caffeine around inhaler time helps you differentiate between medication‑induced tremor and caffeine‑related jitteriness.
When you do indulge in a glass of wine, opt for low‑sulfite choices and monitor any change in wheezing.
Lastly, schedule a dietary review with your pulmonologist every six to twelve months to fine‑tune both your nutrition and medication regimen.
By aligning your eating habits with the pharmacology of albuterol, you can often shave off unnecessary puffs and enjoy a smoother day‑to‑day life.
October 20, 2025 at 23:33
Dana Yonce
Thanks for the clear checklist, it makes tweaking my meals feel doable 😊
October 21, 2025 at 22:53
Angela Koulouris
You’ve laid out a solid roadmap, and it’s easy to picture a week’s worth of asthma‑friendly meals from it.
I love the idea of a turmeric‑spiced sweet potato stew because the color alone feels like a natural boost.
Pairing salmon with a leafy green side not only hits the omega‑3 and vitamin D targets but also keeps dinner exciting.
The snack suggestion of carrot sticks with hummus is perfect for a quick magnesium kick without any dairy drama.
Remember to keep the food‑symptom log handy; even a quick note on your phone can reveal hidden triggers over time.
Small, consistent changes are the real secret sauce for long‑term breathing comfort.
October 22, 2025 at 22:30
erica fenty
Baseline bronchodilator efficacy can be modulated by dietary sulfite load; histamine intake, acid reflux potential, and systemic inflammation markers are pivotal variables; consider nutrient‑pharmacokinetic synergy. Optimizing macronutrient distribution-lean proteins, polyunsaturated fats, low‑glycemic carbs-may attenuate albuterol tachyphylaxis.
October 23, 2025 at 21:50
Ivan Laney
Look, the United States has the best research on asthma management, and we shouldn't be borrowing half‑baked advice from overseas without proper scrutiny.
Albuterol works the way it does because American pharma followed rigorous FDA pathways, and any claim that a “global diet” will magically fix your breathing is pure marketing fluff.
The real issue is that many people still chow down on processed snack chips loaded with hidden sulfites, completely ignoring the warnings on the label.
High‑histamine foods like aged cheddar or cured salami are staples in many cultures, but they’re also proven triggers for bronchospasm in a large subset of patients.
If you think a single glass of wine can’t affect your lungs, think again-sulfite sensitivity is more common than you realize, and the data from American clinical trials is crystal clear.
Acidic citrus may be touted as vitamin C powerhouses, yet the reflux they provoke can undermine the bronchodilator’s effect within minutes.
The proper approach is to adopt a diet rooted in evidence‑based nutrition: lean proteins, plenty of omega‑3 rich fish, and vegetables that don’t scream “acid.”
Hydration isn’t just a suggestion; it’s a medical necessity, because adequate water volume thins mucus and supports mucociliary clearance.
Tracking your meals isn’t optional-it’s a chore you must accept if you want to reduce reliance on rescue inhalers.
Don’t be fooled by trendy “detox” smoothies; many contain hidden sugars that can spike inflammation pathways.
When you schedule a check‑up, bring your log and demand that your doctor acknowledges the dietary component of asthma control, not just the prescription pad.
In short, respect the science, respect the medication, and cut the junk that sabotages your breathing-nothing else will do.
The American dietary guidelines already emphasize low‑sodium, low‑processed food intake; aligning with them naturally benefits asthma.
If you’re traveling abroad, bring your own albuterol and stick to familiar food choices to avoid unexpected triggers.
Ultimately, personal responsibility and adherence to proven nutritional strategies will keep your airways clear and your inhaler in the drawer.
October 24, 2025 at 21:10
Kimberly Lloyd
Food is more than fuel; it’s a bridge between culture and health, especially for those navigating chronic conditions like asthma.
Embracing omega‑3 rich fish not only honors coastal culinary traditions but also offers a gentle anti‑inflammatory shield for the lungs.
Vitamin D, a sunshine vitamin, reminds us that even a brief walk outside can complement our dietary efforts in maintaining airway resilience.
The bright colors of berries and leafy greens echo the optimism we need to breathe freely each day.
By keeping a humble log of meals and breaths, we turn personal data into a story of progress rather than a list of restrictions.
Let’s celebrate each small victory-whether it’s a night without a rescue puff or a new recipe that satisfies both palate and lungs.
October 25, 2025 at 20:30
Sakib Shaikh
Listen up, asthma warriors, cuz the truth about albuterol and diet is kinda mind‑blowing.
If u keep chowing down on processed chips, u r basically feeding the inflammation monster that loves to choke your airways.
Sulfites are sneaky villains hiding in dried fruits and wine, and they can trigger a full‑blown bronchospasm quicker than u think.
Histamine‑rich cheeses? Yeah, they might taste good but they’re like tiny alarm bells ringing in your lungs.
On the bright side, omega‑3 fats from salmon are like peacekeepers, calming the inflammatory warzone inside your chest.
Vitamin D isn’t just for strong bones; it’s a secret weapon that helps your immune system keep asthmatic flare‑ups at bay.
Don’t forget magnesium-bananas and pumpkin seeds are the underrated heroes that help relax those tight bronchi.
And for the drama lovers, a dash of turmeric in your stew adds a golden glow and a powerful anti‑inflammatory punch.
So stop ignoring the food factor and start treating your diet like the sidekick it deserves to be.
Your lungs will thank you, and you’ll finally breathe easy without the constant puff‑puff drama.
October 26, 2025 at 19:06
Chirag Muthoo
I respectfully acknowledge the detailed analysis provided earlier regarding sulfite and histamine sensitivities.
It is indeed prudent to align dietary choices with evidence‑based recommendations to safeguard bronchodilator efficacy.
Moreover, the suggestion to maintain a comprehensive food‑symptom log aligns with best practices in personalized asthma management.
While cultural dietary preferences vary, the core principle of minimizing processed additives remains universally applicable.
I would also add that regular follow‑up with a respiratory specialist ensures that any nutritional adjustments are appropriately calibrated to medication dosing.
Thank you for highlighting these essential considerations.
October 27, 2025 at 18:26
Lolita Gaela
Incorporating a low‑sulfite, high‑omega‑3 dietary regimen can optimize the pharmacokinetic profile of albuterol by reducing airway hyperresponsiveness.
Clinical data suggest that vitamin D sufficiency modulates Th2-mediated inflammatory pathways, thereby decreasing the frequency of rescue inhaler usage.
Magnesium acts as a natural calcium antagonist in bronchial smooth muscle, facilitating bronchodilation synergistically with β2‑agonists.
Patients should aim for a daily intake of at least 1,000 mg of EPA/DHA combined, sourced from marine or plant‑based oils, to achieve measurable anti‑inflammatory effects.
Continuous monitoring through spirometry and symptom diaries will provide objective feedback on the efficacy of these nutritional interventions.
October 28, 2025 at 17:46
Giusto Madison
Totally agree with the practical meal‑plan vibe you laid out; keeping it simple is the secret sauce.
I’ve been swapping out my usual pizza night for a salmon‑and‑kale bowl and noticed fewer late‑night puffs.
The carrot‑and‑hummus snack is a win‑win, giving both crunch and magnesium without the dairy drama.
Keep the log short and sweet-just a quick note on your phone and you’ll spot patterns faster than you think.
Small consistent tweaks really do add up to big breathing gains.
October 29, 2025 at 17:06
Xavier Lusky
All those “diet tips” are just a way for pharma to keep us buying more meds.
October 30, 2025 at 16:26
Write a comment