Medication Weight Gain Estimator
Expected Weight Change
When to expect changes
Select your medication to see personalized weight management tips.
Why this happens
Many people start a new medication expecting relief from their symptoms-but end up dealing with something they didn’t sign up for: a sudden, unexplained change in appetite. One person might feel constantly hungry, eating more even when they’re not hungry. Another might lose interest in food entirely, skipping meals and losing weight without trying. These aren’t just quirks. They’re real, measurable side effects tied to how drugs interact with your brain and body.
Why Your Appetite Changes When You Take Medicine
It’s not random. Medications affect appetite by targeting specific chemicals in your brain that control hunger and fullness. The main players are serotonin, dopamine, histamine, and ghrelin-the hormone that tells your stomach it’s time to eat. When a drug bumps up or down these signals, your body responds.Take antipsychotics like olanzapine or quetiapine. These drugs block histamine and serotonin receptors in the hypothalamus, the part of your brain that regulates hunger. Studies show that within four weeks, people on these medications can have 15-20% higher ghrelin levels. That means your body thinks it’s starving-even when it’s not. In the first 10 weeks of treatment, patients often gain 4-6 kilograms. That’s not just a few pounds. That’s enough to change how you feel about your health, your clothes, even your confidence.
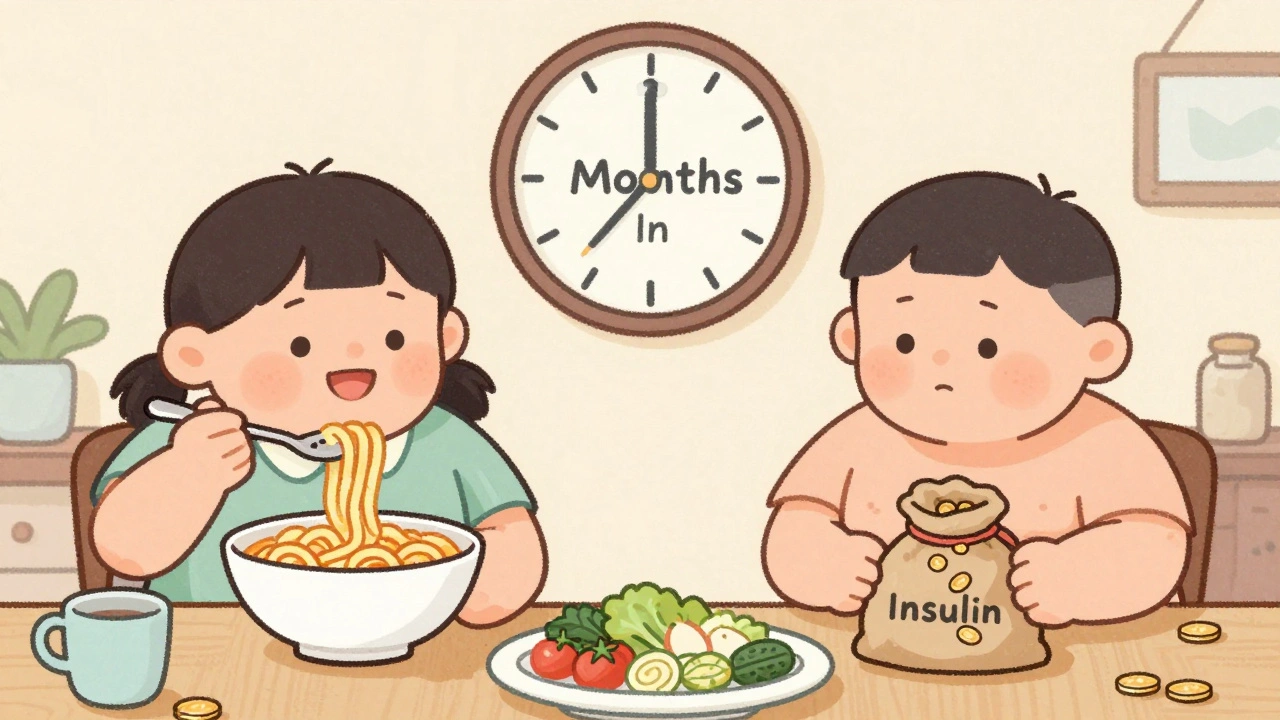
Antidepressants work differently depending on how long you’ve been taking them. In the first few months, drugs like SSRIs can make you feel more in control, reducing impulsive eating. That’s why some people lose a little weight at first. But after a year or more, your brain adjusts. Serotonin receptors become less sensitive. Suddenly, you start craving carbs-bread, pasta, sweets. A third of long-term users report this shift. It’s not willpower. It’s biology.
On the flip side, some medications shut appetite down. Amphetamines, used for ADHD or narcolepsy, boost norepinephrine and dopamine. That suppresses hunger. People on these drugs often eat 300-500 fewer calories a day without even noticing. Diabetes meds like insulin do the opposite. They help your body store glucose as fat, and that can mean 2-4 kilograms of weight gain in just six months. Metformin, another diabetes drug, does the reverse-it often leads to modest weight loss.
Which Medications Are Most Likely to Change Your Appetite?
Not all drugs affect appetite the same way. Some are notorious. Others rarely cause issues. Here’s what the data shows:| Medication Class | Examples | Typical Appetite Effect | Weight Change (6 Months) |
|---|---|---|---|
| Second-gen antipsychotics | Olanzapine, quetiapine, risperidone | Strong increase | +4 to +10 kg |
| Antidepressants | Mirtazapine, amitriptyline, paroxetine | Increase | +2 to +5 kg |
| Antidepressants | Bupropion, vortioxetine | Neutral or decrease | −1 to +0.5 kg |
| Diabetes meds | Insulin, sulfonylureas | Increase | +2 to +4 kg |
| Diabetes meds | Metformin | Decrease | −2 to −3 kg |
| Mood stabilizers | Lithium | Moderate increase | +3 to +5 kg |
| Antihistamines | Diphenhydramine | Mild increase | +1 to +2 kg |
| Appetite suppressants | Topiramate | Strong decrease | −3 to −5 kg |
Some drugs stand out for their extreme effects. Mirtazapine, for example, causes weight gain in 40% of users-more than any other antidepressant. Meanwhile, bupropion is one of the few that can help you lose weight while treating depression. Topiramate, originally an anti-seizure drug, is now used off-label to help counteract weight gain from other meds. In six months, 60% of users lose 3-5 kilograms.
When Weight Gain Isn’t Just About Eating More
It’s easy to blame yourself. “I just ate too much.” But medication-induced weight gain isn’t about overeating. It’s about how your body stores energy.Insulin doesn’t just lower blood sugar-it tells fat cells to hold onto calories. Antipsychotics slow your metabolism. Even if you eat the same amount, your body burns fewer calories. Studies show that within three months of starting olanzapine, resting metabolic rate drops by 5-8%. That’s like losing the ability to burn 100-150 calories a day just by sitting still.
Water retention plays a role too. Some drugs cause your body to hold onto sodium, leading to bloating and scale weight that doesn’t reflect fat gain. That’s why some people panic when the scale goes up-only to find out later that most of it was water, not fat.
And then there’s the emotional side. If you’re on medication for depression or anxiety, your relationship with food can shift. Eating becomes comfort. Or, if you’re feeling numb, you lose interest in meals altogether. These aren’t laziness or lack of discipline. They’re symptoms of how the drug affects your brain.
What You Can Do: Practical Strategies That Work
You don’t have to just accept weight changes as inevitable. There are proven, science-backed ways to manage them-even while staying on your medication.1. Eat protein every 3-4 hours. A snack with 15-20 grams of protein-like Greek yogurt, eggs, or a handful of nuts-keeps your blood sugar steady. That cuts hunger spikes by 40%, according to Harvard Health. No more 3 p.m. sugar crashes or midnight snacking.
2. Swap refined carbs for whole grains. White bread and pasta spike your blood sugar and crash it fast. Whole grains like oats, quinoa, and brown rice digest slower. People who make this switch report feeling full 45 minutes longer after each meal.
3. Drink water before meals. A simple habit: drink two glasses of water 20 minutes before eating. In a group of 200 people using this method, daily calorie intake dropped by 13%. Your stomach fills up faster, and your brain gets the signal to stop eating sooner.
4. Meal prep twice a week. When you’re hungry and tired, you grab what’s easy. That’s when chips, pizza, or fast food win. Prepping meals in advance cuts impulsive eating by 35%. One study showed people who meal prepped ate 200 fewer calories a day than those who didn’t.
5. Move your body, even a little. Resistance training-lifting weights or using resistance bands-builds muscle. Muscle burns more calories at rest. Just two sessions a week can raise your metabolic rate by 50-100 calories a day. That’s the equivalent of walking an extra 15 minutes daily.
6. Practice mindful eating. Put your fork down between bites. Chew slowly. Notice the taste, texture, smell. People who do this reduce portion sizes by 15-20% without feeling hungrier afterward. It’s not magic-it’s rewiring your brain’s response to food.
When to Talk to Your Doctor
Don’t wait until you’ve gained 10 kilograms. The first three months are critical. Eighty percent of significant weight gain happens in that window. The Endocrine Society recommends checking your BMI and waist size every three months if you’re on a medication linked to weight gain.Bring data. Don’t just say, “I’m gaining weight.” Say, “I’ve gained 4 kg in two months since starting olanzapine. I’m eating the same as before, but I’m constantly hungry.” That gives your doctor something concrete to work with.
Ask about alternatives. Is there a weight-neutral option? Vortioxetine, for example, causes only half the weight gain of typical SSRIs. Bupropion might be a better fit than mirtazapine if weight is a concern. Some newer drugs, like KarXT for schizophrenia, show almost no weight gain in early trials.
Never stop or change your medication on your own. Abruptly stopping antipsychotics or antidepressants can cause withdrawal, rebound symptoms, or worse. Tapering takes weeks. Your doctor can help you switch safely-sometimes even adding metformin to counteract weight gain without changing your primary drug.

Real People, Real Results
Reddit threads are full of stories. One man gained 30 pounds on quetiapine in four months. He felt trapped. Then he switched to bupropion, started meal prepping, and lost 15 pounds in six months-without his depression coming back.Another woman on lithium struggled with constant hunger. She started drinking water before meals and swapped white rice for barley. Within three months, her cravings dropped. She lost 5 kg. She didn’t stop her meds. She just changed how she ate.
These aren’t outliers. They’re proof that you have more control than you think. Medications change your biology, but they don’t take away your power to respond.
The Bigger Picture: Why This Matters
Medication-induced weight gain isn’t just a personal issue. It’s a public health problem. In the U.S., 42% of adults have obesity. Experts estimate that 15-20% of those cases are linked to medications. That’s millions of people caught between needing treatment and paying the physical cost.Healthcare is starting to wake up. The FDA now requires drug makers to report detailed weight data for new psychiatric medications. Primary care doctors are screening for weight gain more often-up from 35% in 2015 to 65% today.
And new drugs are coming. Combination therapies like Auvelity (dextromethorphan/bupropion) show only 0.7% average weight gain compared to 2.5% for older antidepressants. Genetic testing is being explored to predict who’s more likely to gain weight on certain drugs. The goal? To match the right medication to the right person-not just by symptoms, but by body type, metabolism, and risk profile.
For now, you’re not alone. And you’re not powerless. Appetite changes from medication are common, predictable, and manageable. With the right tools, support, and a little patience, you can take back control-without giving up the treatment you need.
Why do some medications make me hungry even when I’m not?
Certain drugs, especially second-generation antipsychotics like olanzapine and quetiapine, increase levels of ghrelin-the hormone that signals hunger. They also block histamine and serotonin receptors in the brain, disrupting normal appetite control. This tricks your body into thinking it needs more food, even if you’ve eaten enough. It’s not a lack of willpower-it’s a biological effect.
Can I switch medications if I’m gaining weight?
Yes, but only with your doctor’s guidance. Some antidepressants and antipsychotics are more likely to cause weight gain than others. For example, switching from mirtazapine to bupropion or from olanzapine to a newer option like vortioxetine can reduce weight gain. Never stop your medication abruptly-tapering safely takes weeks. Your doctor can help you transition without risking a relapse.
Does drinking water before meals really help with appetite control?
Yes. In studies, drinking two glasses of water 20 minutes before meals reduced daily calorie intake by an average of 13%. Water fills your stomach, triggering stretch receptors that send fullness signals to your brain. It’s a simple, free, and effective tool-especially useful when medications are making you feel constantly hungry.
Can exercise help counteract weight gain from medication?
Yes, especially resistance training like weightlifting or resistance bands. Building muscle increases your resting metabolic rate by 50-100 calories per day. That means you burn more even when sitting still. Exercise also helps manage stress and mood, which can reduce emotional eating. Two to three sessions a week make a measurable difference.
Is weight gain from medication permanent?
Not necessarily. Many people lose weight after switching medications or adding lifestyle changes. Even while staying on the same drug, strategies like meal prepping, protein-rich snacks, and mindful eating can reverse or slow weight gain. The key is acting early-most weight gain happens in the first six months. The sooner you start managing it, the better your chances of keeping it under control.
Are there any medications that help with weight loss while treating mental health conditions?
Yes. Bupropion (used for depression and smoking cessation) and topiramate (used for seizures and migraines) are known to cause weight loss. Vortioxetine, a newer antidepressant, causes minimal weight gain-only about half as much as older SSRIs. Some doctors now prescribe metformin alongside psychiatric meds to help prevent weight gain. These aren’t magic pills, but they offer better options than before.


Comments
Ariel Nichole
Man, I didn’t realize how much my meds were messing with my hunger until I started meal prepping. Now I keep hard-boiled eggs and almonds in my bag and I’m not raiding the vending machine at 3 p.m. anymore. Small changes, huge difference.
Also, drinking water before meals? Game changer. I used to think it was just a myth until I tried it.
December 11, 2025 at 10:58
john damon
bro i just ate 3 slices of pizza at 2am again 😭 why does my brain think i’m starving??
December 11, 2025 at 20:35
Taylor Dressler
It’s important to distinguish between true hunger and medication-induced cravings. Ghrelin spikes aren’t hunger-they’re neurological noise. Protein-rich snacks work because they stabilize insulin and suppress ghrelin. The 15–20g every 3–4 hours rule isn’t arbitrary; it’s backed by metabolic studies.
Also, water before meals isn’t just about volume-it activates the vagus nerve, which signals satiety faster. It’s physiology, not placebo.
December 12, 2025 at 08:33
Jean Claude de La Ronde
so we’re telling people to drink water and eat protein like it’s 1999? 🤔
Meanwhile, the pharmaceutical industry is selling us pills that make us hungry, then selling us diet plans to fix it. The real question is: why are we still letting this happen?
Also, i just ate a whole bag of chips and now i feel guilty. thanks meds.
December 12, 2025 at 21:39
Katherine Liu-Bevan
I’ve been on mirtazapine for three years. The weight gain was brutal-18 pounds in six months. I started doing resistance training twice a week and swapped white rice for barley. Lost 10 pounds without changing my dose. It’s not about willpower. It’s about working with your biology, not against it.
Also, if you’re feeling numb and skipping meals, that’s valid too. Not everyone gains weight. Some just lose interest. Both are real.
December 14, 2025 at 12:18
Jimmy Kärnfeldt
Reading this felt like someone finally put words to what I’ve been living with. I thought I was lazy. Turns out my brain was just hijacked by olanzapine.
Started meal prepping on Sundays. Now I have grilled chicken, quinoa, and roasted veggies ready to go. No more 10 p.m. cereal binges. I still feel hungry sometimes-but now I know it’s not real hunger. Just my meds being weird.
Also, I’m not alone. That’s the biggest relief.
December 15, 2025 at 15:22
Aman deep
bro i was on lithium and i swear i was hungry ALL the time. like, i’d eat a whole watermelon at midnight and still feel empty 😅
then i started drinking a glass of water before every meal and swapping white bread for sourdough. lost 6 lbs in 3 months without even trying. the body’s wild, man.
also shoutout to the person who said ‘it’s not laziness, it’s biology’-that hit different.
December 16, 2025 at 15:08
Eddie Bennett
the fact that we have to fight our own bodies just to stay healthy because of meds is insane.
i lost 20 lbs on topiramate. then i got switched to quetiapine and gained it all back in 4 months. now i’m stuck between mental stability and looking like a different person.
why is weight gain not listed as a side effect in bold letters on every prescription bottle??
December 17, 2025 at 18:42
Sylvia Frenzel
Oh great. Another article telling people to drink water and eat protein. Groundbreaking.
Meanwhile, the real issue is that doctors don’t care enough to prescribe alternatives. They just hand out olanzapine like candy and expect patients to fix the side effects with kale smoothies.
Wake up. This is systemic neglect.
December 18, 2025 at 23:49
Vivian Amadi
STOP telling people to drink water. That’s not a solution. That’s a Band-Aid on a bullet wound.
People on antipsychotics need to be switched to weight-neutral meds. Not told to chew slower. Not told to meal prep. We’re talking about a 10-pound gain in weeks. This isn’t about ‘habits.’ It’s about dangerous, unmonitored drug use.
Also, your ‘mindful eating’ advice is tone-deaf. When you’re depressed and hungry all the time, mindfulness feels like torture.
December 20, 2025 at 20:30
Jim Irish
Thank you for this comprehensive overview. The data on metabolic rate reduction with olanzapine is particularly compelling. Many clinicians overlook this aspect.
It is also worth noting that cultural factors influence dietary adherence. In some communities, meal prepping is not feasible due to time, cost, or access. Solutions must be adaptable.
December 21, 2025 at 18:36
Mia Kingsley
you guys are all missing the point
what if the real problem is that we’re medicating people who don’t need it in the first place?
what if we just… stopped?
also i once ate a whole cake because my antidepressant made me hungry. so yeah. this is all a scam.
December 22, 2025 at 08:37
matthew dendle
so you’re telling me i’m not a lazy slob i’m just a walking science experiment?
cool. now can i get paid for this?
also i ate 4 donuts this morning and i still feel hungry. thanks for the science bro
December 23, 2025 at 05:37
Monica Evan
My sister’s on risperidone and gained 25 lbs in 5 months. Her doctor said ‘just eat less.’ She cried for hours.
Then we found a psychiatrist who switched her to vortioxetine and added metformin. She lost 14 lbs in 4 months. No more constant hunger. No more shame.
Doctors need to listen. And patients need to demand better options. You’re not broken. Your meds might just be the wrong fit.
December 23, 2025 at 09:37
Aidan Stacey
Just want to say: if you’re reading this and you’re struggling-you’re not failing. Your body is responding to chemistry, not character.
It’s okay to ask for help. It’s okay to ask for a different med. It’s okay to feel like you’re losing yourself.
You’re not alone. And you deserve to feel like yourself again.
- someone who’s been there
December 23, 2025 at 20:42
Write a comment