TL;DR
- Combivir pairs lamivudine with zidoviedine - an older, twice‑daily regimen.
- Newer combos (Truvada, Descovy, Biktarvy) offer once‑daily dosing and better resistance profiles.
- Cost varies: generic Combivir is cheap, but newer branded pills may be covered by subsidies.
- Side‑effects differ - Combivir can cause anemia, while integrase‑based alternatives often cause mild weight gain.
- Choosing the right regimen depends on viral load, kidney health, and insurance coverage.
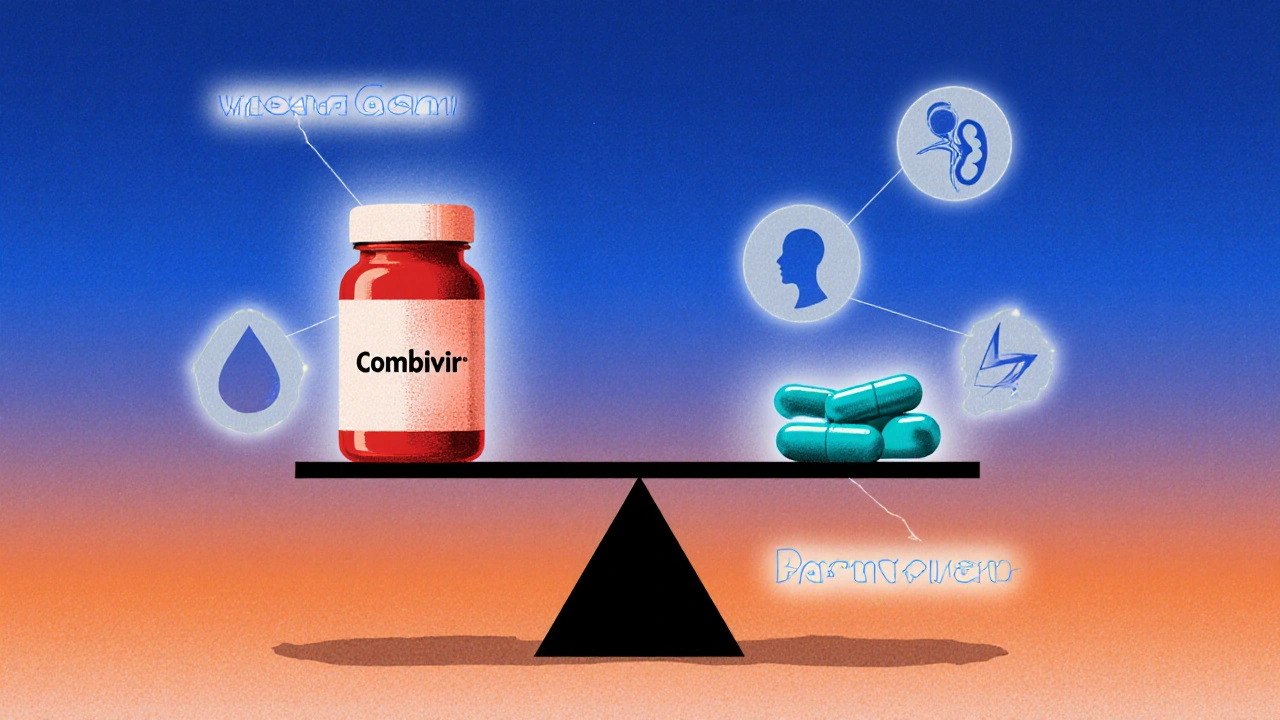
When treating HIV, Combivir is a fixed‑dose combination of lamivudine and zidovudine that has been prescribed since the late 1990s. It works by blocking two steps in the viral replication cycle, keeping the virus at bay when taken twice a day. Over the years, newer single‑tablet regimens have entered the market, promising simpler dosing and fewer side‑effects. This guide lines up Combivir against the most common alternatives, so you can see where it still fits and where newer options pull ahead.
What is Combivir?
Lamivudine is a nucleoside reverse transcriptase inhibitor (NRTI) that mimics the natural building block cytidine, causing premature termination of the HIV DNA chain. Zidovudine (also known as AZT) is another NRTI that works similarly but targets a slightly different step in the reverse‑transcription process. When combined, they provide a double‑hit to the virus, which was especially valuable before the era of integrase inhibitors.
Key attributes of Combivir:
- Dosage: two tablets daily (each tablet contains 150mg lamivudine + 300mg zidovudine).
- FDA approval: 1997.
- Common side‑effects: nausea, headache, anemia, and fatigue.
- Resistance: high barrier when paired with a third agent, but zidovudine resistance can emerge if viral load isn’t suppressed.
Why Compare? The Decision Criteria
Choosing an HIV regimen isn’t just about picking a pill. Clinicians weigh multiple factors:
- Efficacy: ability to achieve and maintain viral suppression (<50 copies/mL).
- Dosing convenience: once‑daily vs twice‑daily.
- Side‑effect profile: impact on blood counts, kidney function, weight, and bone health.
- Resistance barrier: how easily the virus can mutate around the drugs.
- Cost and access: generic availability, government subsidies, private insurance coverage.
With those criteria in mind, let’s stack Combivir against the top five alternatives that dominate Australian prescribing in 2025.
Top Alternatives to Combivir
Each alternative below is presented with its core attributes, so you can compare apples to apples.
- Truvada (emtricitabine/tenofovir disoproxil fumarate) - a once‑daily NRTI backbone widely used in PrEP and HIV treatment.
- Descovy (emtricitabine/tenofovir alafenamide) - newer formulation with lower kidney and bone toxicity.
- Biktarvy (bictegravir/emtricitabine/tenofovir alafenamide) - an integrase‑inhibitor triple‑pill taken once daily.
- Atripla (efavirenz/emtricitabine/tenofovir disoproxil fumarate) - first fixed‑dose single‑tablet regimen, still used where cost is a concern.
- Dolutegravir + Lamivudine - two‑pill regimen that drops zidovudine altogether.
Side‑Effect and Safety Comparison
| Medication | Common Side‑Effects | Serious Risks | Renal Impact | Bone Health |
|---|---|---|---|---|
| Combivir | Nausea, headache, fatigue | Anemia, neutropenia | Low | Low |
| Truvada | Diarrhea, mild nausea | Kidney dysfunction (rare), bone mineral loss | Moderate | Moderate |
| Descovy | Headache, insomnia | Very low renal & bone risk | Low | Low |
| Biktarvy | Weight gain, insomnia | Rare hypersensitivity | Low | Low |
| Atripla | Vivid dreams, dizziness | Neuropsychiatric events, elevated lipids | Low | Low |
| Dolutegravir+Lamivudine | Insomnia, headache | Weight gain, rare liver enzyme rises | Low | Low |
Overall, Combivir’s biggest drawback is anemia, which can be a deal‑breaker for patients with baseline low hemoglobin. The newer tenofovir alafenamide‑based combos (Descovy, Biktarvy) greatly reduce kidney and bone worries, making them preferable for older adults or those with pre‑existing renal disease.
Cost, Generic Availability, and Access in Australia
Cost is often the final arbiter. As of October2025:
- Combivir - generic versions are available; average PBS (Pharmaceutical Benefits Scheme) subsidy brings the out‑of‑pocket cost to around AU$30 per month.
- Truvada - still under patent for many indications; PBS subsidises it for PrEP but not always for treatment, costing roughly AU$80/month.
- Descovy - newer patent, PBS allows limited access for patients with renal concerns; price about AU$100/month.
- Biktarvy - fully subsidised for treatment‑naïve patients; cost about AU$45/month under PBS.
- Atripla - generic emtricitabine/tenofovir became available in 2024, bringing price down to AU$35/month.
- Dolutegravir+Lamivudine - dolutegravir is generic, making the two‑pill combo roughly AU$40/month.
If you’re on a tight budget, Combivir remains the most affordable option, provided you can tolerate its blood‑count effects.
Choosing the Right Regimen - A Practical Checklist
- Baseline labs: Check hemoglobin, creatinine clearance, and bone density. Low hemoglobin nudges you away from Combivir; reduced kidney function favors Descovy or Biktarvy.
- Adherence capacity: Once‑daily pills (Truvada, Descovy, Biktarvy) improve adherence versus twice‑daily Combivir.
- Resistance history: If the virus already carries M184V (lamivudine resistance), Combivir loses potency. Integrase‑inhibitor based combos keep a higher barrier.
- Cost considerations: Verify PBS eligibility. If you qualify for full subsidy, Biktarvy or dolutegravir+lamivudine may be competitively priced.
- Future planning: For patients likely to switch to PrEP or need a single‑tablet regimen for simplicity, starting with Truvada/Descovy eases transition.
In practice, many clinicians start treatment‑naïve patients on Biktarvy or dolutegravir+lamivudine because of their high barrier to resistance and ease of use. Combivir is now mostly reserved for people who have proven tolerance, limited renal issues, and who benefit from the lower drug cost.
Potential Pitfalls and How to Avoid Them
- Missing the anemia signal: Order a full blood count within two weeks of starting Combivir; if hemoglobin drops >2g/dL, consider switching.
- Drug‑drug interactions: Zidovudine can increase toxicity when combined with certain antibiotics (e.g., trimethoprim‑sulfamethoxazole). Review all concomitant meds.
- Adherence missteps: Twice‑daily dosing can lead to missed doses. Use pillboxes and set alarms.
- Renal monitoring for tenofovir combos: Even with alafenamide, check creatinine every six months.
Bottom Line - When Does Combivir Still Make Sense?
If you’re a patient with stable hemoglobin, no significant kidney disease, and you qualify for the PBS subsidy, Combivir can be a cost‑effective backbone when paired with a modern third agent like dolutegravir. However, for most new diagnoses, the trend is moving toward once‑daily, integrase‑based single‑tablet regimens that simplify life and reduce long‑term toxicities.
Frequently Asked Questions
Can I switch from Combivir to a once‑daily regimen without resistance issues?
Yes, most patients can transition to a single‑tablet regimen like Biktarvy or Descovy as long as their viral load is suppressed and resistance testing shows no mutations against the new backbone. A healthcare professional will schedule a brief “wash‑out” period and monitor labs for a few weeks after the switch.
Why does Combivir cause anemia more often than other combos?
Zidovudine interferes with DNA synthesis in rapidly dividing cells, including red‑blood‑cell precursors in the bone marrow. This suppression can lead to a drop in hemoglobin, especially in patients who already have borderline counts.
Is Combivir covered by the PBS for all Australian patients?
Combivir’s generic form is listed on the PBS, so most patients with a valid prescription pay a small co‑payment. However, clinicians must justify its use over newer, subsidised options if those are clinically appropriate.
How do I know if my kidneys can handle tenofovir‑based combos?
A baseline eGFR (estimated glomerular filtration rate) above 60mL/min is generally considered safe for tenofovir disoproxil fumarate (Truvada). If eGFR is between 30‑60, the alafenamide version (Descovy) is preferred because it delivers less drug to the kidneys.
Will switching to a newer regimen affect my viral load monitoring schedule?
No major changes are needed. Continue checking viral load every 3‑6 months as per national guidelines. If the switch is recent, clinicians may add a check at 4‑6 weeks to confirm the new regimen’s effectiveness.


Comments
Richard Sucgang
One must acknowledge the historical significance of Combivir whilst simultaneously recognizing its obsolescence in the modern therapeutic landscape its twice daily dosing scheme simply does not align with contemporary adherence paradigms moreover the anemia risk inherent to zidovudine remains a non‑trivial concern for patients with borderline hemoglobin levels the pharmacokinetic profile pales in comparison to integrase inhibitors which boast superior barrier to resistance while the cost advantage is palpable the clinical trade‑offs are far more consequential
October 3, 2025 at 21:10
Russell Martin
Yo! If you’re lookin for an easy switch just talk to your doc and they’ll hook you up with a once‑daily pill – easier life, less side‑effects!
October 3, 2025 at 21:33
Jenn Zee
It is utterly incomprehensible how anyone could still cling to a regimen that was conceived in the pre‑integrase era and pretend that its antiquated dosing schedule is somehow a virtue. The very premise that twice‑daily administration promotes discipline is a romanticized myth that ignores the stark reality of human forgetfulness. Moreover, the hematologic toxicity profile of zidovudine is not a trivial inconvenience but a manifestation of systemic insult that can precipitate clinically significant anemia, especially in populations already burdened by comorbidities. One must also consider the sociopolitical dimensions of subsidizing a drug that is demonstrably inferior to the newer single‑tablet options that the pharmaceutical industry and public health agencies have championed. When clinicians prioritize cost over efficacy, they inadvertently perpetuate health inequities that are antithetical to the principles of universal care. The resistance barrier, while historically respectable, is eroded in the face of contemporary viral evolution that readily exploits any pharmacologic weakness. It is a moral imperative to transition patients to integrase‑based regimens that offer both a robust genetic barrier and a more forgiving side‑effect profile. The narrative that generic Combivir is a "budget‑friendly" solution conveniently sidesteps the downstream costs associated with managing anemia, fatigue, and reduced quality of life. Additionally, the pharmacodynamic interactions of zidovudine with common prophylactic antibiotics such as trimethoprim‑sulfamethoxazole amplify the risk of bone marrow suppression, a nuance that should dissuade any rational prescriber. From an epidemiological standpoint, simplifying therapy to a single tablet improves adherence metrics across diverse demographic strata, thereby enhancing viral suppression rates at the population level. The data from large cohort studies unequivocally demonstrate that once‑daily integrase inhibitors outperform older NRTI backbones in both virologic and immunologic endpoints. Ethical stewardship of limited healthcare resources mandates that we allocate funding toward therapies that confer maximal benefit, not merely minimal expense. To cling to Combivir in the current era is to willfully ignore a mountain of evidence that advocates for modern regimens. The patient’s voice, often marginalized, repeatedly emphasizes the desire for simplicity and minimal side‑effects, which should be paramount in therapeutic decision‑making. In conclusion, the continued endorsement of Combivir without rigorous justification is anachronistic, clinically indefensible, and ethically questionable.
October 3, 2025 at 22:56
don hammond
Wow, what a nostalgic trip 🤦♂️ – because who doesn’t love a good dose of anemia with their morning coffee? 😂
October 3, 2025 at 23:13
Ben Rudolph
Sure, but not everyone can afford the “new fancy pills”.
October 3, 2025 at 23:30
Traven West
Enough drama – the facts are plain: Combivir is outdated.
October 4, 2025 at 00:20
Jonny Arruda
I get the frustration, but some patients still benefit from the lower cost.
October 4, 2025 at 00:36
Melissa Young
Listen, the US healthcare system is built on cutting‑edge meds not some relic from the 90s – get with the program.
October 4, 2025 at 03:06
SHASHIKANT YADAV
The shift to integrase inhibitors does make sense clinically 👍 and it’s great to see more patients getting that benefit.
October 4, 2025 at 03:23
Ryan Pitt
Exactly! Keep the momentum going, folks.
October 4, 2025 at 03:40
Jami Johnson
From a philosophical standpoint, medication choice reflects a deeper commitment to patient autonomy – when we empower individuals with simpler regimens, we honor their agency and foster trust in the therapeutic alliance.
October 4, 2025 at 05:53
Kasey Krug
While poetic, the practical reality remains: newer pills simply work better.
October 4, 2025 at 06:10
jake cole
This fluff ignores the cold hard data – Combivir is a relic and should be phased out.
October 4, 2025 at 06:26
Natalie Goldswain
i think it's cool that we have options for different budgets.
October 4, 2025 at 08:40
khajohnsak Mankit
In the kaleidoscope of therapeutic possibilities, each regimen paints a distinct hue on the canvas of patient lives, and the brushstroke of simplicity often yields the most vivid masterpiece.
October 4, 2025 at 08:56
Jayant Paliwal
One could argue, with scholarly rigor, that the very existence of an antiquated regimen such as Combivir serves as a pedagogical artifact; it reminds us, in the grand theater of pharmacology, of how far we have traveled from the days of monotherapy and once‑daily dosing is now the gold standard. Yet, let us not dismiss outright the socioeconomic stratifications that dictate drug accessibility – a point that, while often muted in clinical discourse, demands our attention. The interplay between cost‑effectiveness and clinical efficacy is a delicate ballet, and the choreography varies from region to region. In countries where healthcare budgets are constrained, the generic availability of Combivir may still hold pragmatic value, provided that vigilant monitoring of hematologic parameters is instituted. Conversely, in well‑funded systems, the ethical imperative tilts toward prescribing the most tolerable, adherence‑friendly options, thereby reducing long‑term morbidity. Therefore, the decision matrix should incorporate not merely pharmacodynamics but also patient‑centred considerations, such as lifestyle, comorbidities, and personal preferences. Ultimately, the narrative is not binary; it is a spectrum where each point reflects a confluence of clinical evidence, economic realities, and human experience.
October 4, 2025 at 09:13
Write a comment