When your hip starts hurting, it’s easy to assume it’s just from overdoing it at the gym or sitting too long at your desk. But if the pain lingers - especially when you stand up, climb stairs, or twist to put on your shoes - it might not be simple strain. It could be a hip labral tear, early hip arthritis, or both. And here’s the catch: these two conditions don’t just happen one after the other. They feed into each other. Fixing one without addressing the other often leads to the same pain coming back.
What Exactly Is a Hip Labral Tear?
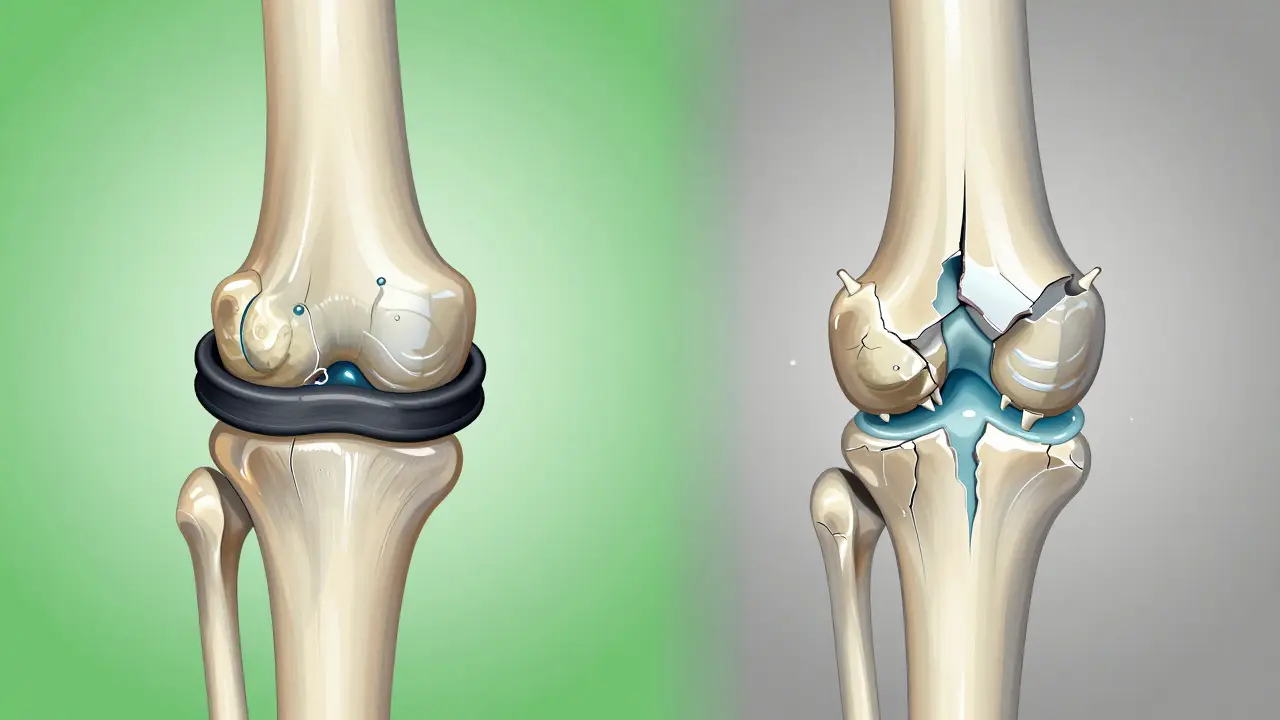
The labrum is a ring of tough, rubbery cartilage that wraps around the socket of your hip joint. Think of it like a gasket sealing a jar - it keeps the ball of your femur snug in the socket, absorbs shock, and helps distribute pressure evenly across the joint. When it tears, that seal breaks. That’s when pain, clicking, or a feeling of the hip “giving way” starts. Labral tears aren’t always from a single injury. In fact, most aren’t. About 78% happen in the front of the hip, often linked to something called femoroacetabular impingement (FAI). This is when the bones of your hip are shaped in a way that causes them to rub against each other over time. There are three types: cam-type (extra bone on the ball of the femur), pincer-type (too much coverage on the socket), and mixed. Cam-type is the most common, making up 64% of cases. Here’s what’s surprising: a 2022 study found that 70-90% of people with FAI already have a labral tear - even if they don’t feel pain. And in people with hip arthritis, over half also have labral damage. The tear isn’t always the cause of the pain. Sometimes, it’s the result.How Arthritis Changes the Game
Hip osteoarthritis (OA) is the slow wearing away of the smooth cartilage that covers the ball and socket. As it progresses, bone grinds on bone. You’ll see this on X-rays as narrowing joint space, bone spurs, and thickening of the bone underneath the cartilage. It’s graded from 0 (normal) to 4 (severe). The problem? Once cartilage starts breaking down, the joint becomes less stable. That puts more stress on the labrum. At the same time, a torn labrum can’t hold synovial fluid properly - the natural lubricant in your joint. Research shows this loss increases contact stress on the cartilage by 92%. So now you’ve got a vicious cycle: arthritis weakens the joint → labrum gets damaged → fluid leaks → cartilage wears faster → arthritis gets worse. And here’s the kicker: many people over 50 have labral tears on MRI scans - but no pain at all. A Yale study found 38% of asymptomatic adults over 50 had them. That means just seeing a tear on an image doesn’t mean it’s the source of your pain. You need to match the imaging with your symptoms.Activity Modification: The Real Secret Weapon
Most people think treatment means either surgery or pills. But the most powerful tool - and often the most ignored - is activity modification. It’s not about resting. It’s about moving smarter. The goal? Reduce pressure on the damaged areas without giving up movement entirely. Studies show that when done right, activity modification alone can reduce pain by 40-60% in mild cases. And for people who avoid surgery, it can delay the need for a hip replacement by 3-5 years. Here’s what actually works:- Don’t flex your hip past 90 degrees. That means no deep squats, no sitting in low chairs, no picking things up from the floor without bending your knees first.
- Avoid twisting your hip inward while bent. That’s the move that tears the labrum - think pigeon pose in yoga, crossing your legs while sitting, or turning sharply in your car.
- Limit continuous weight-bearing to 30 minutes. After that, rest or change position. Set a timer if you have to.
- Switch high-impact to low-impact. Running? Swap it for swimming, cycling, or the elliptical. A Reddit community of 387 hip pain sufferers found 71% could stay active with swimming - only 29% could still run.
What to Avoid - And Why
Some habits make this worse - fast.- Sitting cross-legged. This combines hip flexion and internal rotation - the exact position that stresses a torn labrum. 87% of people in an Arthritis Foundation survey said avoiding this helped.
- Deep lunges. They force the femur into the front of the socket. 92% of respondents stopped them and saw improvement.
- Prolonged sitting without support. If you’re at a desk, your hips are bent at 90-110 degrees. That’s too much. Use a wedge cushion or raise your chair so your hips are slightly higher than your knees.
- Going up and down stairs. Descending stairs puts 3-4 times your body weight through the hip. Use handrails. Take one step at a time. Consider a stairlift if it’s a daily struggle.
When Do You Need More Than Modification?
Activity modification works best for mild to moderate cases - especially if you’re under 60 and have cam-type FAI. But if you’re over 65 and your X-ray shows Grade 3 or 4 arthritis, surgery won’t stop the progression. Total hip replacement becomes the most reliable long-term solution. For people in between - say, 35-60 with a confirmed labral tear and early OA - arthroscopic repair can be very effective. Studies show 85-92% patient satisfaction five years after repair. But debridement (just trimming the tear) only hits 65-75%. Why? Because you’re not fixing the seal - you’re just cutting away the damage. Corticosteroid injections can give you 3-4 months of relief, but repeated use (more than three a year) can damage cartilage. Viscosupplements (like Durolane, approved in 2023) last longer - up to 6 months - but only help about half the people, and the effect fades. The deciding factor? Your bone shape. If your alpha angle (a measurement on MRI) is over 55 degrees, you have cam-type FAI. And if you do, surgical correction + labral repair gives you a 73% better outcome than just physical therapy alone.What Doesn’t Work - And Why
A lot of online advice is misleading.- “Just rest and ice it.” Resting too much leads to muscle weakness, which makes your hip less stable. That speeds up cartilage wear.
- “Do more stretches.” Overstretching a torn labrum can make it worse. Focus on strength, not flexibility.
- “Try acupuncture or magnets.” No solid evidence they change the underlying biomechanics.
- “Wait until it gets worse.” Delaying intervention in active people under 60 often means losing more cartilage. The window to preserve the joint is narrow.

Real-Life Success: The 3-Step Plan
Here’s what a successful plan looks like:- Assess. See a specialist. Get an X-ray and MRI. Ask: Is this FAI? Is there cartilage loss? Is the tear symptomatic?
- Modify. For 4-6 weeks, follow the movement rules: no hip flexion past 90°, no internal rotation while bent, no deep squats or lunges. Use cushions, raise your chair, avoid crossing legs.
- Strengthen. Work with a therapist on hip abductor exercises (side leg raises, clamshells). Aim for 80-100 degrees of hip flexion during training. Build control, not just muscle.
The Invisible Disability
One of the hardest parts isn’t the pain - it’s the misunderstanding. “You look fine,” people say. “Why can’t you just walk normally?” A Hospital for Special Surgery survey found 68% of patients felt this way. You’re not lazy. You’re not exaggerating. Your hip joint is literally breaking down. And you’re managing it with smart movement - not weakness. That’s why education matters. Tell your coworkers. Show your family the movement guidelines. You’re not asking for pity - you’re asking for space to move safely.Looking Ahead
The field is changing fast. Wearable sensors that give real-time feedback on hip position reduced pain episodes by 52% in a 2023 Stanford pilot. New MRI techniques can spot cartilage damage before it shows on X-rays. And the American Academy of Physical Medicine and Rehabilitation now emphasizes “movement quality over quantity.” But the core hasn’t changed: if you have hip pain from a labral tear or arthritis, your best shot at staying active - and avoiding surgery - is understanding how your joint moves, and then changing how you move every day. It’s not about stopping life. It’s about redesigning it - one small adjustment at a time.Can a hip labral tear heal on its own?
No, the labrum doesn’t heal on its own because it has very little blood supply. But symptoms can improve significantly with activity modification and physical therapy. The goal isn’t to make the tear disappear - it’s to reduce stress on it so pain goes away. Many people live pain-free without surgery by avoiding movements that aggravate the tear.
Is walking good for hip arthritis and labral tears?
Yes - but only if you do it right. Walking is low-impact and helps maintain joint mobility. But avoid uneven surfaces, steep hills, or walking for more than 30 minutes at a time without a break. Use supportive shoes. If walking causes pain that lasts more than a few hours afterward, you’re doing too much. Try shorter walks, twice a day, instead of one long one.
Should I stop exercising if I have hip pain?
No - but you need to change what you do. Avoid deep squats, lunges, high-impact sports, and any move that causes a deep ache or clicking in the hip. Replace them with swimming, cycling, elliptical training, or water aerobics. Strength training is still important - focus on glutes, hips, and core with controlled movements. Movement keeps the joint lubricated and muscles strong - both protect your hip.
Can hip arthritis be reversed?
No, once cartilage is worn down, it doesn’t regenerate. But you can slow or even stop its progression. Activity modification, weight management, and targeted strengthening can prevent further damage. In some cases, early intervention with labral repair can preserve cartilage in people with FAI. The key is catching it before the joint collapses.
How do I know if I need surgery?
If you’ve tried 3-6 months of activity modification and physical therapy and still have daily pain, limited mobility, or trouble sleeping, it’s time to see a hip preservation specialist. Imaging showing cam-type FAI (alpha angle >55°) and a symptomatic labral tear strongly suggests surgery will help. But if you’re over 60 with advanced arthritis (Kellgren-Lawrence Grade 3-4), surgery on the labrum won’t fix the main problem - the cartilage loss. In those cases, total hip replacement is often the better long-term option.


Comments
Urvi Patel
Let's be real - most people don't even know what the labrum is. They think yoga is healing when they're literally grinding their hip into oblivion with pigeon pose. The fact that 87% of people who stop crossing their legs feel better? That's not magic. That's biomechanics. Stop treating your body like a yoga prop and start treating it like a precision machine.
December 30, 2025 at 14:33
Deepika D
I want to say thank you for writing this - I’m a physical therapist in Bangalore and I see this every single day. Women in their 40s and 50s come in with hip pain, convinced it’s just ‘aging’ or ‘bad posture’ - but it’s FAI, it’s labral damage, and they’ve been told to ‘just stretch more’ for years. The real win? When they learn to avoid hip flexion past 90 degrees. One client, a schoolteacher, started using a wedge cushion at her desk and within six weeks, she could climb stairs without wincing. No surgery. No pills. Just smart movement. You’re not just giving advice - you’re giving people back their lives. Keep going.
December 30, 2025 at 15:33
Darren Pearson
While the clinical insights presented here are broadly accurate, I must emphasize the methodological limitations of self-reported data from Reddit communities as a primary evidence base. The 71% success rate with swimming, for instance, lacks peer-reviewed validation and introduces significant selection bias. Furthermore, the assertion that activity modification can delay hip replacement by 3–5 years is not supported by longitudinal cohort studies beyond the 2-year mark. A more rigorous approach would involve stratifying patients by alpha angle, joint space width, and activity level - not anecdotal testimonials.
January 1, 2026 at 12:18
Stewart Smith
So let me get this straight - I’m supposed to stop bending over to tie my shoes, avoid stairs, and sit like a robot with my hips slightly higher than my knees… just so I don’t have to get a hip replacement at 55? And you’re telling me this is better than just taking a pill and going about my day? I mean… I guess if I want to live like a museum exhibit labeled ‘Human in Preservation Mode,’ sure. But can I at least still do push-ups? Asking for a friend who’s not ready to become a walking posture correction poster.
January 2, 2026 at 09:11
Retha Dungga
life is pain 🤕 but pain is also a teacher 🌱
your hip is screaming not because you're weak but because you've been listening to the wrong voices
stop chasing flexibility
start building stability
the body knows what it needs if you just shut up and listen 🙏✨
sleep with a pillow between your knees 🌙
you're not broken you're just misaligned 💫
January 2, 2026 at 10:19
Jenny Salmingo
I had this pain for years. Thought it was just from sitting too much. Then I started using a raised toilet seat and putting a pillow between my legs at night. No more pain when I wake up. I didn’t even know these little things mattered. Now I tell everyone. It’s not fancy. It’s not expensive. But it works. You don’t need surgery to feel better.
January 4, 2026 at 01:52
Aaron Bales
Activity modification works because it reduces shear forces on the joint. No magic. Just physics. Avoid flexion + internal rotation = less labral stress. Simple. Do this for 6 weeks. If no improvement, get a proper MRI and alpha angle measurement. Stop guessing. Start measuring.
January 4, 2026 at 09:47
linda permata sari
My mother was told she’d need a hip replacement by 50. She’s 62 now. Still walks two miles a day. No surgery. Just modified everything. No deep squats. No cross-legged sitting. Raised her chair. Used a cane when she was tired. People thought she was being dramatic. But she didn’t care. She didn’t want to be the woman who couldn’t play with her grandkids. This isn’t just medical advice - it’s a love letter to your future self. 💔➡️❤️
January 6, 2026 at 06:32
Write a comment