Sickle Cell Trait vs Malaria Risk Calculator
This calculator shows the relative malaria risk based on your hemoglobin type. The sickle cell trait (HbAS) provides partial protection against severe malaria, but does not eliminate risk. Always follow standard malaria prevention measures.
Your Malaria Risk Assessment
Malaria Severity Risk
This shows your relative risk compared to the baseline (HbAA).
Risk Reduction
Recommendations
Key Takeaways
- Sickle cell anemia and malaria share a centuries‑old evolutionary relationship.
- People with one sickle‑cell gene (trait) have a measurable survival edge in malaria‑endemic regions.
- The protective effect stems from altered red‑cell properties that hinder the malaria parasite’s life cycle.
- Understanding this link helps shape screening programs, vaccine trials, and treatment strategies.
- Both carriers and patients still need malaria prevention; the advantage only applies to the heterozygous state.
Why These Two Diseases Keep showing up together
When you read headlines about sickle cell disease or malaria, they often appear in the same paragraph. That’s not a coincidence - it’s a classic example of sickle cell anemia and malaria influencing each other’s prevalence for thousands of years. The story blends genetics, parasite biology, and public‑health policy, and it gives us a rare glimpse of natural selection in action.
What is Sickle Cell Anemia?
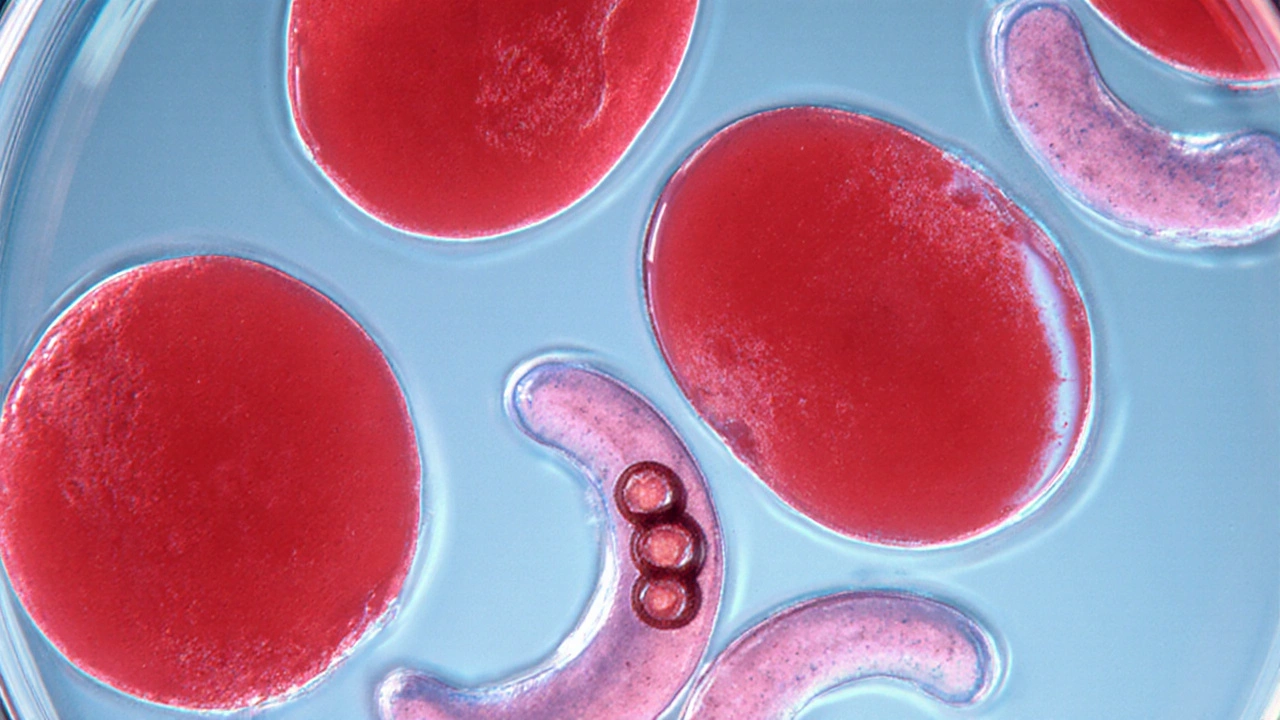
Sickle Cell Anemia is a genetic blood disorder caused by a single‑letter mutation (GAG → GTG) in the beta‑globin gene. This mutation produces hemoglobin S (HbS), an abnormal form of hemoglobin that polymerizes when oxygen levels drop, forcing red blood cells into a rigid, crescent shape. The misshapen cells break down quickly, leading to chronic anemia, pain crises, and organ damage.
Globally, about 300000 babies are born with sickle cell disease each year, most in sub‑Saharan Africa, the Middle East, and parts of India. The disease follows an autosomal recessive pattern: two copies of the HbS gene cause full‑blown anemia, while one copy produces the sickle‑cell trait (carrier state).
What is Malaria?
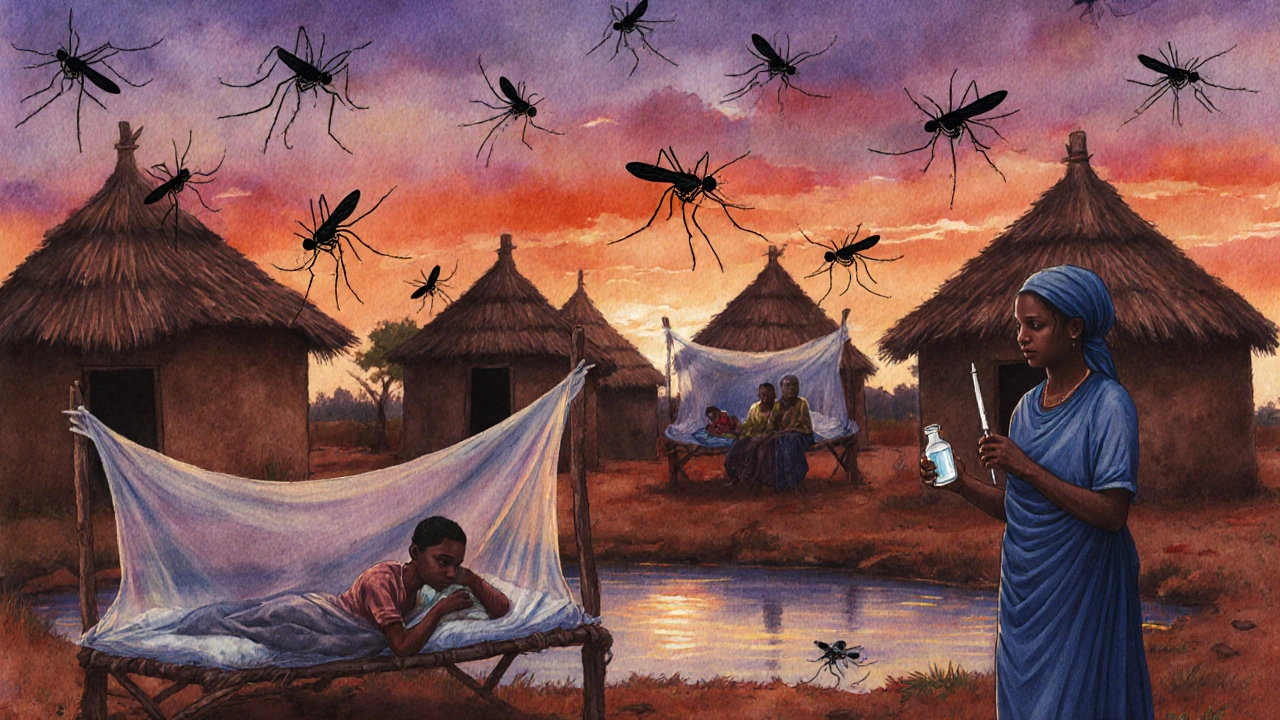
Malaria is a mosquito‑borne infection caused by parasites of the genus Plasmodium. The most lethal species, Plasmodium falciparum, infects red blood cells, triggering fever, chills, anemia, and in severe cases, organ failure or death.
According to the World Health Organization (WHO), there were an estimated 241million malaria cases and 627000 deaths worldwide in 2023, with more than 90% of fatalities occurring in children under five in Africa.
Evolutionary Link: The Heterozygote Advantage
The concept of a "heterozygote advantage" (also called balanced polymorphism) explains why a harmful gene can persist in a population. In the case of sickle‑cell trait, having one HbS allele (carrier) provides a survival benefit against severe malaria, while two copies cause disease.
Early field studies in the 1950s, notably by Dr. J. B. S. Haldane and later by Prof. Anthony Allison, showed that mortality from malaria in carriers was roughly half that of non‑carriers. This selective pressure kept the HbS allele at frequencies as high as 10-20% in some African regions, despite its deadly effect in homozygotes.
How the Mutation Messes with the Parasite
Three main mechanisms explain the protective effect:
- Impaired Parasite Growth: The polymerized HbS creates a less hospitable environment inside red cells, slowing Plasmodium replication.
- Increased Removal of Infected Cells: Sickled cells are more readily cleared by the spleen, reducing parasite load.
- Enhanced Immune Signaling: The altered cell surface triggers a stronger innate immune response, alerting the body to infection earlier.
These mechanisms are most effective when only one HbS gene is present. In double‑gene individuals, the severe sickling outweighs any anti‑malaria benefit.
Epidemiological Evidence from the Field
Modern cohort studies in Ghana, Tanzania, and Kenya consistently show that children with the sickle‑cell trait have a 30-50% lower incidence of severe malaria compared with children with normal hemoglobin (HbAA). A 2022 meta‑analysis of 22 trials reported a pooled odds ratio of 0.45 for severe malaria in carriers.
Conversely, people with full‑blown sickle cell disease remain vulnerable. Their chronic anemia and splenic dysfunction actually increase the risk of severe malaria complications, underscoring that the protective advantage is strictly limited to heterozygotes.
Clinical Implications: What Doctors Need to Know
For clinicians in malaria‑endemic areas, genetic screening for the sickle‑cell trait is standard practice before prescribing certain drugs (e.g., primaquine) that can trigger hemolysis in carriers. The screening also helps estimate community‑level malaria risk.
Patients with sickle‑cell disease require aggressive malaria prophylaxis-often daily chloroquine or intermittent preventive treatment-because their protective effect disappears. Vaccination with the RTS,S/AS01 (Mosquirix) vaccine is recommended for all children, regardless of genotype, but carriers may derive added benefit from the vaccine’s partial immunity.

Public‑Health Perspective: From Screening to Policy
The WHO’s 2024 malaria elimination strategy explicitly mentions hemoglobinopathies as a factor in tailoring interventions. Countries with high HbS frequencies adopt combined approaches:
- Nationwide newborn screening for sickle‑cell disease and trait.
- Targeted distribution of insecticide‑treated bed nets to high‑risk zones.
- Community education about the limited nature of the protective trait.
- Integration of malaria chemoprevention into sickle‑cell care programs.
These policies aim to reduce malaria morbidity while also improving outcomes for sickle‑cell patients, who often face barriers to care.
Comparison Table: Malaria Susceptibility by Hemoglobin Type
| Genotype | Hemoglobin Type | Malaria Severity | Typical Clinical Outcome |
|---|---|---|---|
| HbAA | Normal | High risk of severe disease | Standard treatment, higher hospitalization rates |
| HbAS | Sickle‑cell trait (carrier) | 30‑50% reduced risk of severe disease | Often mild or asymptomatic infections |
| HbSS / HbSC | Sickle‑cell disease | Increased risk due to anemia & splenic dysfunction | Higher mortality; requires aggressive prophylaxis |
What This Means for You
If you or a family member lives in a malaria‑endemic area, a simple blood test can tell you whether you carry the HbS gene. Knowing your status helps you make informed choices about:
- Choosing the right antimalarial medication.
- Adhering to bed‑net use and indoor residual spraying.
- Scheduling regular health check‑ups, especially if you have sickle‑cell disease.
Remember, the protective effect is modest and only applies to carriers - it does not replace standard malaria prevention.
Next Steps & Resources
For deeper learning, consider these reputable sources:
- World Health Organization (WHO) - annual malaria reports and hemoglobinopathy guidelines.
- Centers for Disease Control and Prevention (CDC) - factsheets on sickle‑cell disease and malaria prevention.
- National Institutes of Health (NIH) - research articles on heterozygote advantage.
Local health departments often run free screening events; checking their calendars can save you a trip to the clinic.
Frequently Asked Questions
Does having sickle‑cell trait mean I’m immune to malaria?
No. Carriers have a lower chance of severe disease, but they can still get infected and spread the parasite. Prevention measures remain essential.
Can people with sickle‑cell disease take the malaria vaccine?
Yes. The RTS,S/AS01 vaccine is safe for all hemoglobin types and is recommended for children in endemic regions, including those with sickle‑cell disease.
Is genetic testing for the sickle‑cell trait covered by health insurance?
In many countries with public health programs, newborn screening is free. In other settings, private insurance often covers the test because it informs malaria‑prevention strategies.
Why do carriers still need bed nets if they’re partially protected?
The protection is only partial and varies by parasite load and individual health. Bed nets block mosquito bites, which is the most reliable way to avoid infection.
What other hemoglobinopathies show a similar malaria connection?
Alpha‑thalassemia and certain hemoglobin C variants also confer modest protection, though the evidence is strongest for the sickle‑cell trait.

Comments
John Hoffmann
The sickle‑cell trait reduces parasite replication by altering the hemoglobin polymerization process. In heterozygous individuals, red cells sickle under low oxygen tension, which impedes Plasmodium development. Moreover, the spleen removes these misshapen cells more efficiently, lowering parasite load. Consequently, carriers experience a statistically significant decline in severe malaria cases.
October 14, 2025 at 13:26
Sharath Babu Srinivas
🩸🦟 The protective mechanism starts at the molecular level, where HbS changes the red‑cell interior. This environment slows the parasite’s life cycle, and the immune system clears sickled cells faster. 🌍 Populations with high HbAS frequencies thus see lower mortality from Plasmodium falciparum infections. 😊
October 18, 2025 at 16:12
Halid A.
From an epidemiological perspective, the heterozygote advantage associated with sickle‑cell trait has been quantified in numerous cohort studies. The reduction in severe malaria incidence ranges between thirty and fifty percent, depending on regional transmission intensity. This statistic underscores the evolutionary pressure maintaining the HbS allele in endemic zones.
October 22, 2025 at 18:57
Brandon Burt
When you look at the data from West African villages, the pattern emerges with a clarity that is hard to ignore.
Children who inherit a single HbS allele tend to survive malaria outbreaks that decimate their peers.
The physiological changes in their erythrocytes create a hostile niche for Plasmodium falciparum.
Sickling under hypoxic stress leads to premature removal of infected cells by the spleen, a process that is markedly more efficient than in normal red cells.
Additionally, the altered membrane proteins trigger innate immune pathways that accelerate the clearance of parasites.
Researchers have measured parasite densities in carriers and found them to be consistently lower than in non‑carriers.
This reduction translates into fewer clinical episodes of high fever, anemia, and cerebral malaria.
Consequently, the mortality curves for HbAS individuals dip noticeably compared with the HbAA baseline.
However, the protective effect is not absolute; carriers can still contract malaria and contribute to transmission cycles.
The public health implication is that reliance on the genetic advantage alone is insufficient for disease control.
Preventive strategies such as insecticide‑treated nets, indoor residual spraying, and chemoprevention remain essential.
In fact, some health ministries incorporate hemoglobin screening into malaria control programs to fine‑tune intervention distribution.
The interplay between genetics and environment exemplifies a classic case of balanced polymorphism.
It also raises ethical considerations regarding newborn screening and counseling in regions where both diseases are prevalent.
Overall, the evidence supports a nuanced view: the sickle‑cell trait offers a significant but partial shield against severe malaria, demanding integrated approaches for optimal outcomes.
October 26, 2025 at 20:43
Gloria Reyes Najera
i think people forget that sickle cell trait is not a super vaccine it just helps a bit and ye still need nets the gene stuck around cuz it gave our ancestors an edge dont ignore that
October 30, 2025 at 23:28
Gauri Omar
Picture a battlefield inside every tiny red cell, where the mutant hemoglobin swings the sword of destiny against the relentless malaria parasite! The trait turns the invader’s own weapons against it, a ruthless but glorious defense that has shaped entire continents!
November 4, 2025 at 02:14
Willy garcia
That's a solid summary of the protection mechanism.
November 8, 2025 at 05:00
zaza oglu
Wow! The genetics saga reads like an epic saga where tiny heroes battle unseen foes-truly awe‑inspiring!
November 12, 2025 at 07:45
Vaibhav Sai
Did you ever imagine that a single amino‑acid swap could turn our blood into a secret weapon?!! It's amazing how evolution writes its own thriller!!
November 16, 2025 at 10:31
Lindy Swanson
Some folks hype the sickle‑cell trait like it’s a miracle cure, but the reality is far messier and the narrative often glosses over the suffering of homozygotes.
November 20, 2025 at 13:17
Amit Kumar
😊 Absolutely, the story is complex, yet it also shows nature’s clever tricks! 🌱 Let’s celebrate the resilience while we keep pushing for better prevention!
November 24, 2025 at 16:02
Crystal Heim
The oversimplification is dangerous it masks the true burden on patients
November 28, 2025 at 18:48
Sruthi V Nair
If we view disease as a teacher the trait teaches us about trade‑offs in survival
December 2, 2025 at 21:34
Mustapha Mustapha
Indeed, embracing both the science and the humanity behind these genes guides us toward smarter health policies.
December 7, 2025 at 00:19
Write a comment