Substance Use & STI Risk Calculator
Assess Your STI Risk
Select substances you've used in the past 30 days and indicate your usage frequency to calculate your relative STI risk.
How this works: Based on data from the Journal of Adolescent Health and CDC studies, this calculator estimates your relative STI risk compared to non-users. The risk factors are multiplied together to give you a combined risk multiplier.
What to do: High-risk users should prioritize STI testing every 3-6 months, consider PrEP if applicable, and reach out to local harm reduction services.
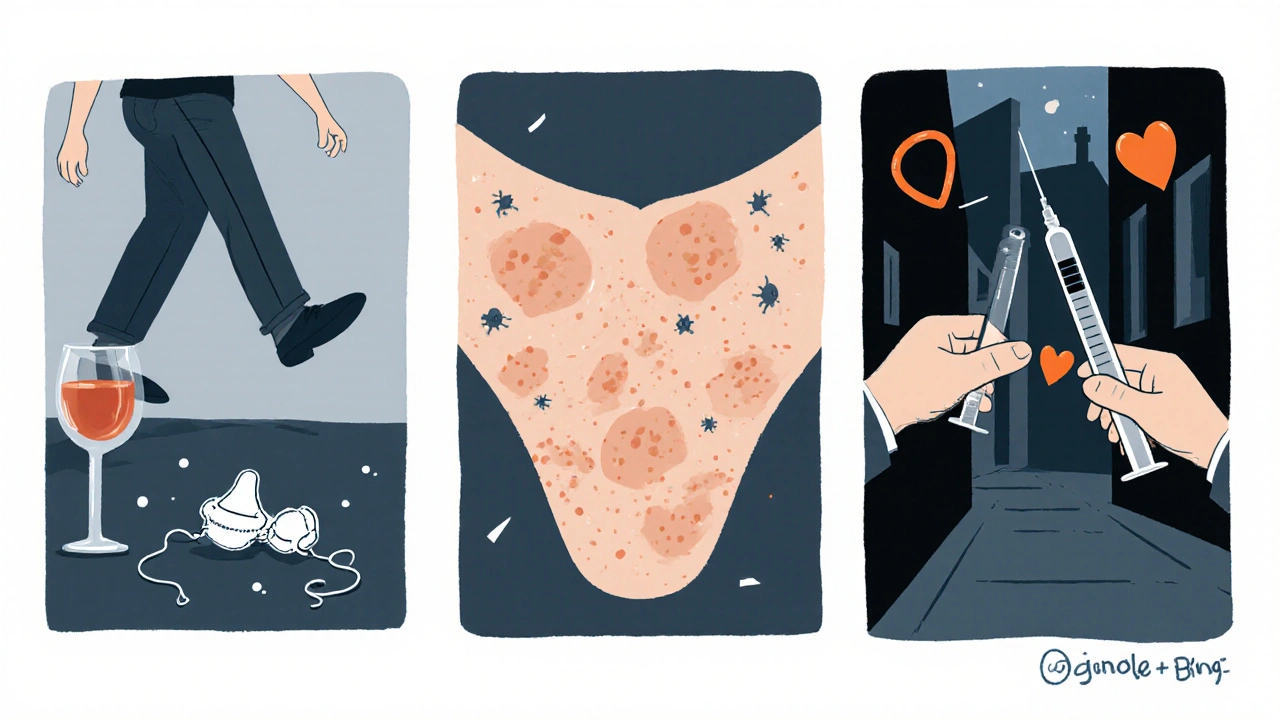
When substance abuse is defined as the harmful or hazardous use of psychoactive substances-including alcohol, illicit drugs, and misused prescription meds-its impact goes far beyond liver damage or overdose. One of the hidden yet serious consequences is a sharp rise in the likelihood of contracting Sexually Transmitted Infections (STIs). This article untangles why that happens, which substances are the biggest culprits, and what practical steps can cut the double danger.
What Counts as Substance Abuse?
Substance abuse covers a wide spectrum:
- Alcohol - binge drinking or daily heavy use.
- Illicit drugs - heroin, cocaine, methamphetamine, and the like.
- Prescription misuse - taking opioids, benzodiazepines, or stimulants without medical guidance.
According to the 2024 World Health Organization report, roughly 270 million people worldwide use substances in a way that harms their health. The same study links substance use to risky sexual behavior in 62 % of surveyed individuals.
Understanding Sexually Transmitted Infections
Sexually transmitted infections are infections spread primarily through sexual contact. Major bacterial STIs include Chlamydia and Syphilis. Viral STIs feature prominently with HIV, human papillomavirus (HPV), and herpes simplex virus (HSV). In 2023 the CDC recorded over 2.5 million new STI cases in the United States alone, a 15 % rise from the previous year.
Why Substance Use Fuels STI Transmission
Three core mechanisms explain the link:
- Impaired judgment - Alcohol and many drugs lower inhibitions, leading to unprotected sex or multiple partners.
- Physiological changes - Certain substances, like methamphetamine, can cause genital sores that make infection easier.
- High‑risk settings - Needle sharing among injectors, sex work, and crowded living environments increase exposure.
For instance, a 2022 study in the Journal of Adolescent Health found that teens who reported binge drinking were 2.8 times more likely to test positive for chlamydia within six months.
STI Risk by Substance Type
| Substance | Typical Use Pattern | Associated STI Risk Increase | Key Mechanism |
|---|---|---|---|
| Alcohol | Binge drinking (≥5 drinks/occasion) | 1.9‑fold | Lowered condom use, multiple partners |
| Heroin (injecting) | Daily injection | 2.5‑fold | Needle sharing, co‑occurring sex work |
| Methamphetamine | Frequent binge | 3.3‑fold | Sexual stamina boost → longer sessions, sores |
| Cocaine (snorting) | Weekend binge | 2.1‑fold | Increased libido, impaired decision‑making |
| Prescription Opioids (misuse) | High‑dose daily | 1.7‑fold | Depressed immune response, risky encounters |
Populations Where the Overlap Is Most Apparent
Certain groups face a double burden:
- Incarcerated individuals - Drug use behind bars pairs with limited access to condoms, driving outbreaks of HIV and syphilis.
- People experiencing homelessness - Survival sex and limited hygiene amplify infection rates.
- Sex workers - Substance use is often a coping tool, yet it raises the chance of unprotected encounters.
- LGBTQ+ youth - Higher reported rates of meth use and concurrent STI diagnoses.
Targeted outreach in these settings shows the biggest return on public‑health investment.
Prevention: From Harm Reduction to Screening
Effective prevention blends behavioral, biomedical, and structural tactics.
Harm‑Reduction Services
Programs like Needle Exchange sites not only provide clean syringes but also distribute condoms and pamphlets about STI testing. A 2023 evaluation in Chicago recorded a 27 % drop in new HIV cases among participants.
Biomedical Tools
- PrEP (pre‑exposure prophylaxis) cuts HIV risk by up to 99 % when taken consistently.
- HPV vaccination guards against the strains that cause most cervical cancers and genital warts.
Regular Screening
Because many STIs are asymptomatic, routine testing every 3‑6 months is vital for people who use substances. Rapid point‑of‑care tests now deliver results in under 15 minutes, enabling immediate treatment.
Education and Counseling
Motivational interviewing, a client‑centered counseling style, has proven effective at reducing risky sex among opioid‑dependent patients. Combining counseling with medication‑assisted treatment (MAT) yields the lowest relapse and STI rates.

Treatment Pathways: Integrated Care Models
When substance use and an STI co‑occur, siloed treatment often fails. Integrated clinics that offer both addiction services and sexual‑health care close that gap. For example, the Boston Health Care for the Homeless Program reported a 34 % increase in STI treatment adherence after adding on‑site buprenorphine prescribing.
Key components of a successful integrated model include:
- Co‑located services - patients can see a counselor and a sexual‑health clinician in the same visit.
- Shared electronic health records - ensure no duplicate testing and track medication interactions.
- Peer support - individuals with lived experience help reduce stigma.
Key Takeaways
- Substance abuse dramatically raises the chance of acquiring STIs through impaired judgment, physiological effects, and high‑risk environments.
- Alcohol, heroin, methamphetamine, cocaine, and misused opioids each carry a distinct risk profile.
- Populations such as incarcerated people, the homeless, sex workers, and LGBTQ+ youth need targeted harm‑reduction and screening.
- Prevention works best when it combines needle exchange, PrEP, vaccination, regular testing, and counseling.
- Integrated care settings that treat addiction and sexual health together improve outcomes for both conditions.
Frequently Asked Questions
Does occasional drinking increase STI risk?
Even occasional binge drinking can lower inhibitions enough to skip condom use. Studies show a 1.5‑fold increase in STI diagnoses after just one binge episode in the past month.
Can using methamphetamine cause physical changes that make infection easier?
Yes. Meth can cause skin lesions and genital sores, which serve as entry points for bacteria and viruses, raising the odds of chlamydia, gonorrhea, and HIV transmission.
Is PrEP recommended for people who inject drugs?
Absolutely. The CDC advises PrEP for anyone at substantial HIV risk, including people who share needles or have condom‑less sex while using drugs.
How often should someone who uses substances get tested for STIs?
Every three to six months is a good rule, or after any change in sexual partners or drug‑use patterns. More frequent testing may be needed for those in high‑risk settings.
Do needle‑exchange programs reduce STI rates?
Yes. By providing clean syringes, condoms, and health education, they cut both HIV and bacterial STI transmission among people who inject drugs.


Comments
Monika Bozkurt
Integrated care models that co‑locate addiction treatment and sexual‑health services dramatically cut comorbidity rates; by synchronizing electronic health records clinicians can track both substance‑use patterns and STI testing outcomes, leading to earlier interventions and improved adherence.
October 19, 2025 at 15:35
Catherine Viola
Beyond the surface statistics, it's crucial to recognize that coordinated data sharing may be compromised by undisclosed agendas; without transparent oversight, the purported benefits of integrated clinics risk becoming a façade for profit‑driven surveillance.
October 19, 2025 at 15:45
sravya rudraraju
When we think about the intersection of substance use and STI risk, the first thing to acknowledge is that the two are not merely correlated but often causally entwined, creating a feedback loop that amplifies health hazards for individuals and communities alike.
For instance, binge drinking lowers inhibition, making condom use less likely, while stimulants like methamphetamine can induce genital sores that act as portals for pathogens.
These physiological changes are compounded by the environments where drug use frequently occurs-crowded shelters, sex work venues, and needle‑exchange sites-where the opportunity for unprotected encounters multiplies.
Addressing this requires a multipronged strategy that goes beyond simple education; it demands the integration of harm‑reduction services with robust sexual‑health screening programs.
Needle‑exchange programs, when equipped with condoms and informational leaflets, have demonstrated measurable drops in both HIV and bacterial STI incidence.
Similarly, providing PrEP to people who inject drugs or engage in high‑risk sex can slash HIV transmission risk by up to 99% when adherence is maintained.
Vaccination against HPV further protects against a suite of cancers and warts, underscoring the benefit of biomedical prophylaxis in tandem with behavioral interventions.
Regular testing every three to six months ensures that asymptomatic infections are caught early, reducing the likelihood of onward transmission and long‑term complications.
Motivational interviewing, as a client‑centered counseling approach, has shown efficacy in curbing risky sexual behavior among opioid‑dependent patients, especially when paired with medication‑assisted treatment such as buprenorphine.
Integrating these services under one roof-so that a patient can see an addiction counselor and a sexual‑health clinician in the same visit-eliminates barriers, streamlines care, and improves adherence to both treatment regimens.
Shared electronic health records facilitate seamless coordination, preventing duplicate testing and flagging potential drug‑interaction concerns that could affect STI treatment efficacy.
Peer support networks, drawing on individuals with lived experience, further destigmatize both substance use and STI testing, fostering a community of trust and mutual accountability.
Targeted outreach to high‑risk groups-including incarcerated populations, the homeless, sex workers, and LGBTQ+ youth-maximizes public‑health impact by focusing resources where they are needed most.
In practice, programs like the Boston Health Care for the Homeless have reported a 34% rise in STI treatment adherence after adding on‑site buprenorphine prescribing, illustrating the power of integrated care.
Ultimately, reducing STI prevalence among people who use substances is not a matter of morality but of evidence‑based public‑health strategy, requiring coordinated, compassionate, and comprehensive action at every level of the system.
October 19, 2025 at 16:10
Ben Bathgate
While the long‑form analysis is thorough, the practical takeaway is simple: combine clean needles and condoms in outreach kits, and the infection numbers will start to dip.
October 19, 2025 at 16:18
Ankitpgujjar Poswal
Stop waiting for perfect programs and start pushing aggressive harm‑reduction now; every day without clean syringes and condom distribution is a day we lose lives to preventable infections.
October 19, 2025 at 16:43
Bobby Marie
Clean gear saves lives.
October 19, 2025 at 16:53
Christian Georg
Quick tip: if you’re in a program that offers rapid HIV testing, grab the result on the spot and get treatment immediately – it cuts the transmission chain and feels great 😊.
October 19, 2025 at 17:16
Christopher Burczyk
It bears emphasizing that timely point‑of‑care diagnostics, when coupled with immediate linkage to care, constitute a cornerstone of effective public‑health response, as supported by recent epidemiological data.
October 19, 2025 at 17:26
Write a comment