Every year, over 1.5 million people in the U.S. suffer preventable harm from medication errors. Many of these errors happen because someone didn’t double-check the medication name, the strength, or the dosage form before giving or taking a drug. It’s not always a mistake by a doctor or pharmacist - sometimes, it’s a missing decimal, a confusing abbreviation, or a label that’s too small to read. But you don’t have to be a clinician to help prevent these errors. Whether you’re picking up a prescription, managing your own meds, or helping a loved one, knowing how to verify these three critical details can save a life.
Start with the Medication Name: Avoid Look-Alike, Sound-Alike Confusion
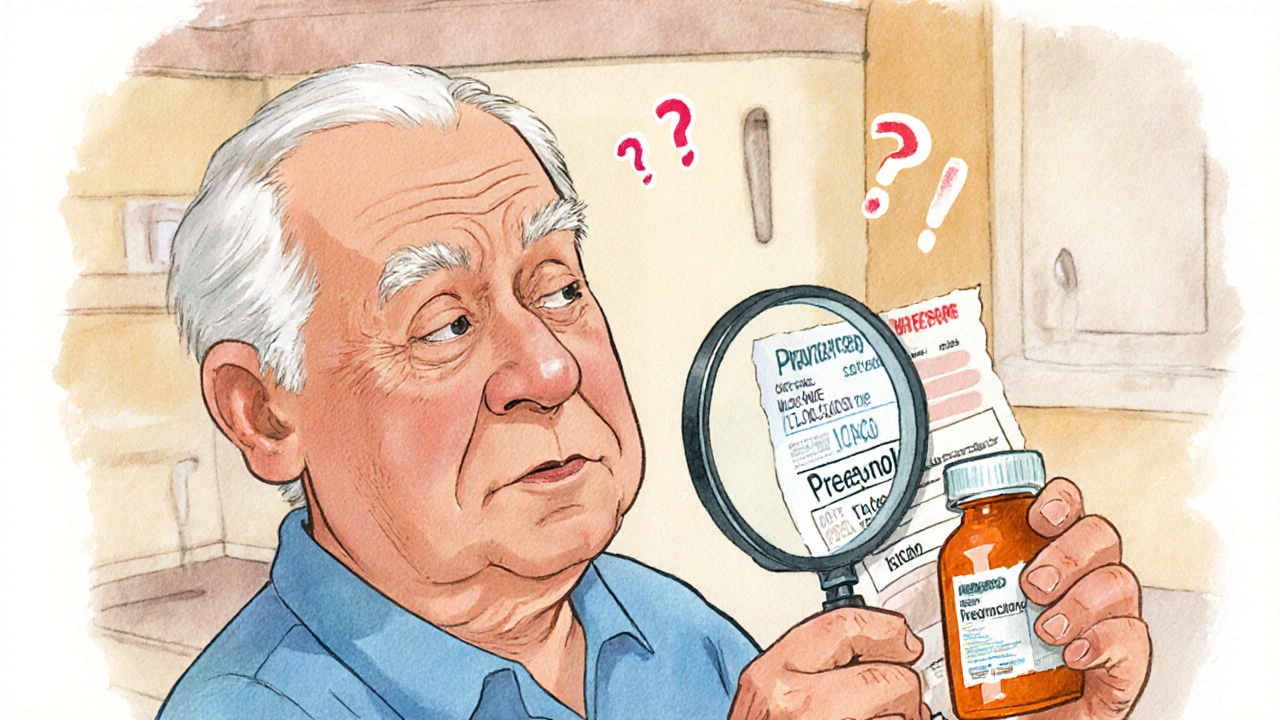
Medication names can be deceptively similar. Prednisone and Prednisolone sound almost identical. Hydralazine and Hydroxyzine are easy to mix up. These aren’t typos - they’re dangerous look-alike, sound-alike (LASA) drug pairs. The FDA and the Institute for Safe Medication Practices (ISMP) have documented hundreds of cases where patients got the wrong drug because of this.Here’s how to catch it: Always read the full name out loud. Don’t just glance. Say it slowly: "P-R-E-D-N-I-S-O-N-E." Compare it to the prescription slip, the pharmacy label, and the pill bottle. If you see an abbreviation like "MS" on a chart, ask: "Does that mean magnesium sulfate or morphine sulfate?" In emergency rooms, "MS" is still misread as morphine 12% of the time, even though it’s banned. That’s enough to cause a fatal overdose.
Healthcare systems use "Tall Man" lettering to help - like predniSONE and predniSOLONE - to highlight the differences. If you’re looking at an electronic record or printed label and don’t see this formatting, ask why. You have the right to see the full, unambiguous name.
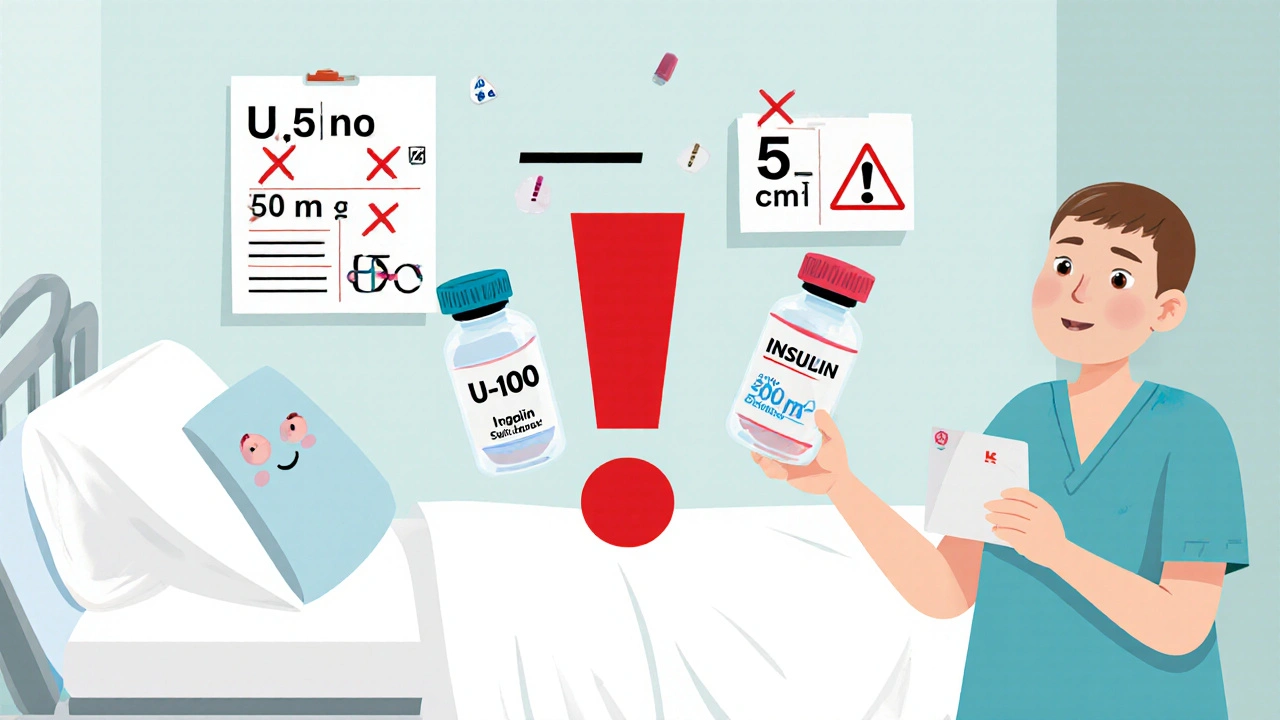
Verify the Strength: The Decimal That Could Kill
Strength tells you how much active drug is in each unit. A tiny mistake here can be deadly. Take insulin: U-100 means 100 units per mL. U-500 is five times stronger. If someone mistakes one for the other, they could inject five times the dose. That’s not hypothetical - it happens.Another common error? Missing zeros. ".5 mg" looks like "5 mg" if the decimal is smudged or hard to see. Always write and read doses with a leading zero: 0.5 mg, never .5 mg. The FDA and ISMP both require this. Same with "mcg" - never write "μg" or "ug." The "μ" symbol looks like "u," which can be mistaken for "mg," leading to a 1,000-fold overdose.
For injectables, avoid ratios. Epinephrine should be labeled as 0.1 mg/mL, not 1:10,000. The latter is outdated and confusing. Even trained staff misread ratios. A 2015 ISMP report found 236 errors linked to epinephrine concentration confusion between 2010 and 2015. Always confirm the strength matches the original prescription. If the bottle says 5,000 units/mL but the order says 50 units/mL, stop. Don’t assume it’s a typo. Ask.
Check the Dosage Form: Oral vs. Topical, Tablet vs. Capsule
The dosage form tells you how the medication is meant to be taken. A tablet isn’t interchangeable with a liquid. A patch isn’t a pill. Yet, people mix them up all the time.One Reddit user shared how a nurse almost gave an oral medication meant for skin use - a topical cream - by mouth. The label didn’t clearly state "for external use only." The patient could’ve suffered serious internal damage. Another common error: crushing a time-release capsule because it’s hard to swallow. That can release the entire dose at once, causing overdose.
Always check the form: Is it a tablet, capsule, liquid, patch, inhaler, or injection? If the prescription says "capsule" but you get a tablet, ask why. If it says "suspension" but you get a tablet, don’t take it. Some medications are only absorbed properly in certain forms. For example, extended-release metformin tablets must be swallowed whole. Breaking them ruins the slow-release mechanism.
Also, watch for changes in form after a refill. Pharmacies sometimes substitute generics with different shapes or colors. That’s legal - but you need to know what you’re getting. Don’t assume the pill looks the same just because the name is the same. Use a pill identifier app or ask the pharmacist to confirm the form matches the prescription.
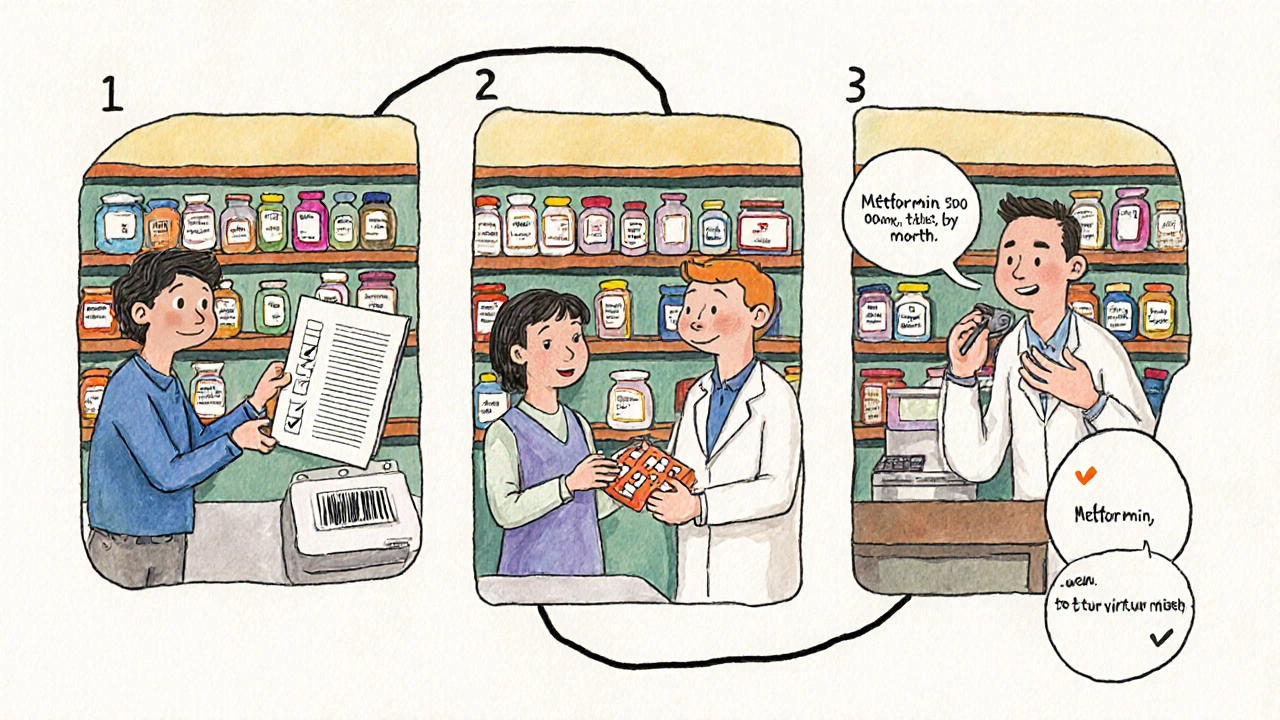
The Three-Point Verification Rule
Experts agree: verification must happen at three key moments - not just once.- When you receive the order - whether it’s from a doctor, an e-prescription, or a handwritten note. Check for completeness: Is the drug name full? Is the strength included with units? Is the dosage form specified? If any piece is missing, don’t proceed.
- When you prepare the medication - whether you’re a pharmacist counting pills or a caregiver opening a blister pack. Match the physical medication to the prescription. Use the "Five Rights": right patient, right drug, right dose, right route, right time.
- Just before administration - right before you swallow it, inject it, or apply it. Read the label again. Say it out loud: "This is metformin 500 mg, tablet, taken by mouth, once daily."
This isn’t just for professionals. If you’re giving meds to an elderly parent or a child, follow these steps. You’re not being overly cautious - you’re being smart. A 2023 Mayo Clinic study found that using a "four-eyes" rule - two people verify high-risk meds - cut errors by 94%.
Use Technology Wisely - But Don’t Trust It Blindly
Electronic health records and pharmacy systems help. Barcode scanning reduces dispensing errors by 83%. Systems like Epic and Cerner flag look-alike names and calculate doses automatically. But here’s the catch: automation bias is real.Doctors and nurses sometimes ignore red flags because the system says "approved." A 2020 study by The Joint Commission found that 18% of errors happened because clinicians trusted the computer too much. If the screen says "Heparin 5,000 units/mL" but the vial says "50 units/mL," don’t click "confirm." Double-check the vial. Trust your eyes more than your screen.
Also, not all systems are equal. Community pharmacies and nursing homes often use older tech. In 2023, only 38% of long-term care facilities used barcode systems. If you’re in one of those settings, your vigilance becomes even more critical.
What to Do When Something Doesn’t Add Up
If you spot a mismatch - a different color pill, a missing unit, a confusing abbreviation - don’t hesitate. Say something. Ask: "Can we confirm this?"Use the "read-back" method. After the pharmacist or nurse tells you the medication, repeat it back: "So this is lisinopril 10 mg, tablet, once daily?" If they hesitate or correct you, you just prevented a mistake.
Keep a written list of all your medications - name, strength, form, and why you take it. Update it every time something changes. Bring it to every appointment. Many errors happen because providers don’t have the full picture.
Common Pitfalls to Avoid
- Never use abbreviations like "U" for units - write "units"
- Never use "cc" for milliliters - use "mL"
- Never assume the dose is correct just because it’s on a label - verify against the original order
- Never ignore a change in pill appearance - even if the name is the same
- Never skip the final check before taking or giving a drug
High-alert medications - like insulin, heparin, opioids, and potassium chloride - require extra care. These are the drugs that cause the most serious harm when given wrong. If you’re handling one, treat it like a loaded gun. Double-check. Triple-check.
What’s Changing in Medication Safety
The FDA is pushing for digital drug labels that machines can read - meaning future prescriptions will include machine-readable codes for name, strength, and form. AI tools are being tested to scan pill bottles and catch label errors with 99% accuracy. But these are tools, not replacements for human attention.Right now, the most effective safety tool is still you - the person holding the pill bottle, reading the label, asking the question. No algorithm can replace your eyes, your voice, and your willingness to pause and verify.
What should I do if the medication name on my prescription doesn’t match the label?
Stop. Don’t take the medication. Call the pharmacy or your prescriber immediately. Mismatches can happen due to transcription errors, generic substitutions, or labeling mistakes. Always confirm the full name, strength, and dosage form before use. If the pharmacy made a mistake, report it - this helps improve safety for everyone.
Why is it dangerous to use "U" for units on medication labels?
The letter "U" can be mistaken for the number "0" or the letter "V," especially in handwritten or poorly printed labels. This has led to 10-fold dosing errors with insulin and other medications. The FDA and ISMP banned "U" in 2006. Always write out "units" in full to avoid confusion.
Can I rely on my pharmacy’s electronic system to catch all errors?
No. While electronic systems help flag many errors - like look-alike names or incorrect doses - they’re not perfect. They can miss unclear handwriting, outdated drug names, or unusual combinations. They also create alert fatigue, where users ignore warnings because they’re too frequent. Always verify the physical medication yourself before taking it.
What’s the difference between strength and dosage form?
Strength tells you how much active drug is in each unit - like 500 mg of amoxicillin. Dosage form tells you how it’s delivered - tablet, capsule, liquid, or injection. Both are essential. Taking the wrong form (like crushing a time-release tablet) can be dangerous, even if the strength is correct.
How can I make sure I’m taking my medication correctly?
Use the three-point verification rule: check the name, strength, and form when you receive the prescription, when you prepare it, and right before you take it. Write down your meds with all three details. Ask your pharmacist to explain what each one does. If something looks or feels different, ask why. Your attention is the last line of defense.

Comments
JAY OKE
Just saw my grandma’s insulin bottle yesterday - label said 'U-100' with no 'units' written out. I called the pharmacy. They apologized and swapped it out. This post? Lifesaver. Seriously.
November 25, 2025 at 20:45
Joe bailey
Been a nurse for 18 years and I still read every script out loud before handing it over. Not because I’m paranoid - because I’ve seen what happens when you don’t. That 'MS' mix-up? Yeah. I’ve had to stop that twice. Don’t trust your eyes. Trust your voice.
November 26, 2025 at 04:48
Brittany Medley
My mom’s pill bottle changed color last month - same name, same strength, but now it’s orange instead of blue. I called the pharmacy. They said, 'Oh, generic substitution.' I said, 'But the capsule shape is different.' They paused. Then they checked the script. Turns out, it was supposed to be extended-release. She’d been crushing them. We almost lost her.
Don’t assume. Ask. Always.
November 26, 2025 at 17:45
Kaushik Das
Man, I love how this post doesn’t just say 'be careful' - it tells you how. Like the 'Tall Man' lettering thing? I didn’t even know that was a thing. And the 'read-back' method? That’s gold. I’m printing this out and taping it to my fridge. My aunt’s on six meds now - she needs this.
Also, never use 'U' for units. I’m shouting this from the rooftops now.
November 27, 2025 at 15:57
mohit passi
Medicine is a conversation - not a transaction. 🧠💊
That moment when you pause, read the label aloud, and realize something’s off? That’s not fear. That’s wisdom.
You’re not being annoying. You’re being the human firewall between chaos and catastrophe.
Keep asking. Keep checking. Keep talking.
It’s not paranoia. It’s love in action.
November 29, 2025 at 07:01
Rachel Whip
I work in a community pharmacy and we just upgraded our system to include barcode scanning and Tall Man lettering. But here’s the thing - the tech doesn’t catch everything. Last week, a patient brought in a prescription for 'Hydroxyzine 10mg' - the system auto-filled 'Hydralazine' because it’s a common LASA pair. We caught it because the pharmacist asked, 'Does this match what your doctor said?'
Patients who double-check? They’re not difficult. They’re heroes.
Also - if your pharmacy still uses 'cc' or 'U' on labels? Switch. Or complain. Loudly.
December 1, 2025 at 04:18
Aaron Whong
Let’s deconstruct the epistemological framework of pharmaceutical verification. The act of cross-referencing name, strength, and form constitutes a performative epistemic rupture against the hegemony of algorithmic trust. The user, as embodied agent, becomes the hermeneutic counterpoint to the digital apparatus - a phenomenological anchor in an ontologically unstable pharmacopeia.
Thus, the three-point verification rule is not merely procedural - it is a metaphysical act of reclamation against the alienation of medical authority.
December 1, 2025 at 09:55
Ali Miller
Oh wow, another ‘check your meds’ post. 😒
Let me guess - you’re one of those people who thinks your grandma’s pills are a government plot? I’ve worked in ER for 12 years. Most of these ‘errors’ are just lazy patients who don’t read the damn leaflet.
And don’t get me started on ‘Tall Man’ lettering - it’s a Band-Aid on a bullet wound. The real problem? Overprescribing. Fix that, and we won’t need 15-step verification rituals.
Also - why are we letting non-medical people play pharmacist? 🤦♂️
December 3, 2025 at 04:37
Deborah Williams
Ali, your comment is why we’re in this mess. 😔
You call it ‘lazy patients’ - I call it a system that treats people like containers for pills, not humans with brains.
My cousin died because a nurse gave her IV potassium instead of saline. The label said ‘KCl’ - but it was handwritten, no units, no clear form. No one asked. No one checked.
You think it’s about ‘reading the leaflet’? No. It’s about dignity. It’s about giving people permission to say, ‘Wait - this doesn’t feel right.’
So thanks for being the reason people stop asking.
December 5, 2025 at 03:32
Cynthia Springer
Can someone explain why 'mcg' is preferred over 'μg'? I’ve seen both in my prescriptions and I’m confused. Is it just about font compatibility? Or is there a deeper reason?
December 5, 2025 at 04:17
james thomas
Y’all are losing it. Next thing you know, we’ll need a notary to sign off on Tylenol.
My uncle takes 12 pills a day and he’s fine. He doesn’t read labels. He just swallows.
And don’t even get me started on ‘read-back’ - that’s what happens when you let lawyers run hospitals.
Stop scaring people. Most meds are fine. Chill out.
December 6, 2025 at 15:22
Sanjay Menon
How quaint. You’re all treating medication like a sacred rite while ignoring the root cause: pharmaceutical capitalism. The system is designed to overwhelm. Look-alike names? That’s not an accident - it’s a profit engine. Generic manufacturers know consumers won’t notice the difference, so they optimize for cost, not clarity.
And you? You’re just cleaning up the mess while the CEOs cash in.
Check your pills? Sure. But ask yourself - why is this even a thing in 2025?
December 6, 2025 at 21:21
Marissa Coratti
As someone who has spent the last decade advocating for patient safety protocols in both acute care and long-term facilities, I must emphasize that the three-point verification rule is not merely a recommendation - it is a non-negotiable standard of care that aligns with the Joint Commission’s National Patient Safety Goals and the Institute of Medicine’s seminal report, To Err Is Human. The statistical reduction in medication errors - 94% - when a dual-verification process is implemented is not anecdotal; it is empirically validated across multiple peer-reviewed studies conducted between 2018 and 2023. Furthermore, the FDA’s 2006 ban on the abbreviation 'U' for units was not a bureaucratic formality, but a direct response to over 1,000 documented adverse events attributable to misinterpretation of the symbol. In clinical settings where barcode scanning and electronic prescribing are absent - which, regrettably, remains the case in approximately 62% of skilled nursing facilities - the responsibility falls squarely upon the individual to act as the final and most reliable safety checkpoint. This is not about fear. It is about accountability. It is about honoring the trust placed in us by those who are vulnerable. Do not underestimate the power of a simple question: 'Can we confirm this?'
December 7, 2025 at 10:01
Asia Roveda
And yet… no one’s talking about the real enemy: the FDA’s slow rollout of digital labels. We’re still using paper prescriptions in 2025? Come on. This is why we have errors. The system is broken. It’s not patients being ‘careless’ - it’s the government and Big Pharma keeping things archaic because change costs money. I’ve seen my sister’s meds changed twice because the pharmacy didn’t update their database. They blamed ‘human error.’ I blame corruption.
And now you want me to read every label out loud? Fine. But I’m not just checking the pill - I’m checking the system.
December 9, 2025 at 02:40
Write a comment