When someone you love is taking multiple medications, it’s easy to assume they’re managing it all on their own. But the truth is, medication adherence is one of the biggest challenges in home care-and it’s not something most people can handle alone. Nearly half of all adults over 65 take five or more prescriptions. That’s not just a list-it’s a daily puzzle of timing, dosages, interactions, and side effects. And when confusion sets in, missed doses, overdoses, and dangerous drug interactions follow. The good news? Involving family or caregivers doesn’t just help-it saves lives.
Why Caregivers Are Essential in Medication Management
You don’t need to be a nurse to make a difference. Family members and caregivers are often the ones who notice when a pill goes missing, when someone skips a dose because they feel fine, or when a new side effect shows up. According to the Caregiver Action Network, 83% of U.S. caregivers are already managing some part of their loved one’s medication routine. But many do it without training, tools, or clear guidance. That’s where things go wrong. Medication errors at home cause over 125,000 preventable deaths in the U.S. each year. Half of those errors happen because the person taking the meds-or the person helping them-doesn’t have a clear, updated list of what’s being taken, why, and when. Hospitals discharge patients with stacks of new prescriptions, but no one explains how they fit together. That’s where caregivers step in-not as replacements for doctors, but as the missing link between the clinic and the kitchen table.Start with a Complete Medication List
Before you do anything else, build a master list. Not a scribble on a napkin. A real, detailed, up-to-date record. The Agency for Healthcare Research and Quality (AHRQ) says every medication entry needs at least 17 key details:- Brand name and generic name (e.g., Lisinopril, sold as Zestril)
- Exact dosage (e.g., 10 mg, not just "one pill")
- Time of day to take it (e.g., "8 AM with breakfast")
- How to take it (with food? on empty stomach? swallow whole?)
- Purpose (e.g., "lowers blood pressure," "reduces inflammation")
- Prescribing doctor’s name and contact
- Pharmacy name and phone number
- When it was started
- Any known side effects
- Drug interactions to watch for
- Refill status and next due date
- Number of pills left in the bottle
- Special instructions (e.g., "avoid grapefruit")
- Whether it’s a new prescription or a change
- Reason for any change
- Who to call if there’s a problem
- Emergency red flags (e.g., "if missed, call doctor immediately")
Use Tools That Actually Work
Paper lists are a start, but they’re not enough. You need systems that reduce human error. Here’s what works:- 7-day AM/PM pill organizers: These simple plastic boxes cut missed doses by 37% in clinical studies. Use them for meds taken twice a day. Don’t use them for pills that need to be taken at odd hours (like 2 AM)-they’re not flexible enough.
- Electronic pill dispensers: Devices like Hero Health or MedMinder automatically dispense pills at set times, play voice reminders, and alert caregivers if a dose is skipped. In trials, they reduce missed doses by 62%.
- Smartphone apps: Apps like Medisafe or Round Health send push notifications, track refills, and let you share status with up to five family members. Users report a 45% improvement in adherence compared to paper logs.
- Voice assistants: Alexa or Google Home can be programmed to say, "It’s 8 AM. Take your blood pressure pill." For people with memory issues, this simple reminder cuts missed doses by 37%, according to a University of Pittsburgh study.
Build Routines Around Existing Habits
People remember routines, not schedules. That’s why linking medication times to daily habits works better than alarms alone. This is called "habit stacking," and it’s backed by the National Institute on Aging.- Take your morning pill right after brushing your teeth.
- Take your evening pill when you sit down for dinner.
- Take your afternoon pill after you check your mail.

Know the Red Flags
Not all missed doses are equal. Some meds are dangerous if skipped. Create a "medication red list"-a separate note you keep near the pill organizer or on the fridge. Include:- Insulin (missed doses can cause diabetic emergencies)
- Anticoagulants like warfarin or apixaban (missed doses raise stroke risk)
- Heart medications like beta-blockers or digoxin (can cause irregular heartbeat)
- Seizure meds like levetiracetam (missed doses can trigger seizures)
- Steroids like prednisone (sudden stop can cause adrenal crisis)
Work With the Pharmacist
Your pharmacist is the most accessible medication expert you’ll ever meet. Unlike doctors, they’re available without an appointment, often for free. Ask them these four questions every time you pick up a new prescription:- What time should this be taken relative to meals?
- Are there foods, alcohol, or other meds I should avoid?
- What should I do if I miss a dose?
- When should I expect to feel the effect?
Attend Appointments Together
If you’re helping manage medications, go to the doctor’s appointments. Bring the master list. Write down what the doctor says. Ask questions. A 2023 AARP survey found that 89% of caregivers who attended appointments reported better understanding of the medication plan. That’s not luck-it’s because doctors assume patients know more than they do. You’re not interrupting-you’re filling the gap.Watch for Polypharmacy Risks
Taking five or more medications is common-but not harmless. The American Geriatrics Society’s Beers Criteria lists 30 drugs that are risky for older adults. These include certain sleeping pills, antihistamines, and muscle relaxers that increase fall risk. Ask your doctor: "Is this still necessary?" and "Can any of these be stopped?" A 2023 study found that 45% of adults over 65 on five or more meds had a 50% higher risk of falling and a 30% higher chance of hospitalization. Regular reviews every 3-4 months can cut inappropriate prescriptions by 22%.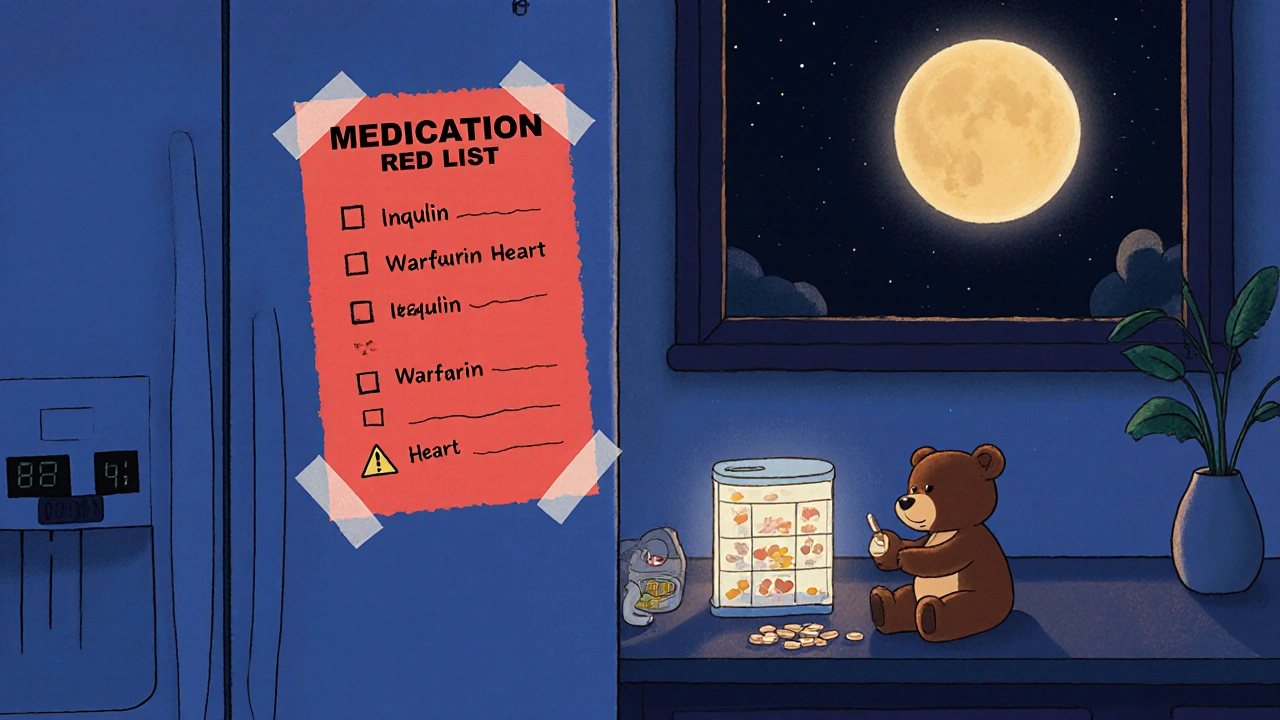
Prepare for Transitions
The biggest risk for medication errors happens when someone leaves the hospital. In fact, 50-60% of all home medication errors occur in the first week after discharge. Here’s how to prevent it:- Before discharge, ask for a written list of all meds-new, changed, and stopped.
- Call the pharmacy to confirm the list matches what’s being dispensed.
- Review the list with your loved one at home, one pill at a time.
- Call the doctor if anything doesn’t make sense.
Watch for Burnout
Managing medications is stressful. In fact, 42% of caregivers say it’s their most stressful task. If you’re feeling overwhelmed, you’re not alone. Don’t wait until you’re exhausted to ask for help.- Ask other family members to share the load-maybe one handles refills, another does the reminders.
- Use home care agencies that offer medication support. 73% now include training for this.
- Check if your local Area Agency on Aging offers caregiver respite programs.
- Join a support group. Reddit’s r/caregivers and the Caregiver Action Network have thousands of people sharing real tips.
What’s Next? Technology Is Getting Smarter
The future of medication support is already here. Smart pills with sensors (like Proteus Discover) can tell if a pill was swallowed and send a notification to caregivers. AI-powered assistants are being added to Alexa Care Hub and Google Nest. By 2027, 65% of caregiver support systems are expected to use AI to predict missed doses before they happen. But tech doesn’t replace human care. It just makes it easier. The best system still needs a person who cares enough to notice when something’s off.Can I use a pill organizer for all medications?
No. Pill organizers work well for pills taken twice a day, like morning and evening doses. But they’re not safe for medications that need to be taken at irregular times, like insulin or blood thinners that require dose adjustments based on lab results. Always check with the pharmacist before putting any medication in a pill box.
What if my loved one refuses to take their meds?
Don’t force it. Try to understand why. Is it because of side effects? Cost? Confusion? Talk to the doctor about alternatives. Sometimes switching from a pill to a liquid, or from a daily dose to a weekly patch, makes a big difference. Never stop or change meds without medical advice.
How often should I review medications with the doctor?
At least every 3-4 months if your loved one takes four or more medications. For those on five or more, quarterly reviews are critical. Ask the doctor: "Is every medication still needed?" and "Are there any that can be stopped safely?" This reduces the risk of harmful interactions and side effects.
Are there free services to help with medication management?
Yes. Medicare Part D offers free Medication Therapy Management (MTM) for those taking 8+ Part D drugs with 3+ chronic conditions. Most major pharmacies like CVS and Walgreens also offer free consultations with pharmacists. Local Area Agencies on Aging often provide free caregiver support, including medication reviews.
What should I do if I find a pill I don’t recognize?
Don’t guess. Take the pill to a pharmacy and ask the pharmacist to identify it. Many pharmacies have pill identifier tools. You can also use the National Library of Medicine’s Pillbox tool online. Never throw out or take an unknown pill without confirmation.

Comments
King Over
This is solid. Pill organizers work for some meds but not all. Learned that the hard way when my grandma took her blood thinner in one and ended up in the ER. Always check with the pharmacist.
November 20, 2025 at 20:11
Johannah Lavin
I cried reading this. 🥹 My mom’s on 12 meds and I thought I was doing okay until I saw how much I was missing. The 7-day organizer + Alexa reminders changed everything. She actually says she feels less scared now. Thank you for writing this. 🙏
November 21, 2025 at 15:19
Ravinder Singh
In India, we don’t have access to Hero Health or smart apps, but we use the old-school method: sticky notes on the fridge, family calls at 8 AM and 8 PM, and the local pharmacist who knows everyone’s meds by heart. Simple works. Also, never underestimate the power of a good chai and a chat while handing out pills. 😊
November 23, 2025 at 03:06
Russ Bergeman
This article is way too long. You’re overcomplicating it. Just make a list. Use a phone alarm. Done. Why do we need 17 details? Who has time for this? Also, why are we trusting pharmacists? They’re just selling pills.
November 24, 2025 at 00:03
Dana Oralkhan
I’ve been doing this for my dad for 3 years. The red list? Game changer. I printed it in 18pt font and taped it to the fridge next to the milk. He still forgets, but now I know when to panic. Also, don’t be afraid to say ‘I need help’ - it’s not weakness, it’s strategy.
November 24, 2025 at 06:55
Jeremy Samuel
Lol who even uses pill organizers anymore? I just put all the pills in a jar and shake it when I feel like it. Works fine. Also, doctors are just in it for the money. Why do you think they keep prescribing more?
November 25, 2025 at 20:56
Destiny Annamaria
OMG I just started helping my aunt and I was SO lost. This post is literally my new bible. I’ve already made the master list, set up Medisafe, and asked my pharmacist if we could do MTM. She said yes! And now I’m telling EVERYONE. This is life-saving info, not just advice.
November 27, 2025 at 19:38
Ron and Gill Day
This is performative caregiving. You’re not saving lives-you’re just checking boxes. The real problem? The system is broken. Pharmacies don’t care. Doctors don’t listen. And now you’re just making caregivers feel guilty for not doing enough. Great. Just great.
November 28, 2025 at 20:12
Alyssa Torres
I used to think I was doing a good job until my mom had a fall because she skipped her beta-blocker. Now I have a color-coded system: red = emergency, yellow = important, green = routine. I also record voice memos for her when she’s confused. She says she feels like she’s not alone anymore. 💛
November 30, 2025 at 12:38
Summer Joy
I’m so tired of people acting like this is a ‘love language’. My mom’s meds are a nightmare and I’m burnt out. No one talks about how it feels to be the human pharmacy. I’m not a nurse. I’m not a doctor. I’m just a daughter who needs a nap.
December 1, 2025 at 12:25
Shiv Karan Singh
This is all Western nonsense. In our village, we just give the pills and say ‘God will protect’. No apps, no lists, no alarms. Why are we trusting technology more than faith? And why are we wasting money on these gadgets? 🤔
December 2, 2025 at 00:34
Ravi boy
I read this while eatin breakfast. My uncle’s on 8 meds and I just started helpin him. I dunno if I got all the details right but I made a list on my phone notes. It’s messy but it’s there. Also, the pharmacist at my local shop gave me free advice. He’s a legend.
December 2, 2025 at 00:54
Matthew Karrs
This is all a scam. The FDA knows these meds are dangerous. They’re just letting it happen because Big Pharma profits. Why do you think they push 5+ prescriptions on seniors? It’s not about health-it’s about control. You’re being manipulated.
December 2, 2025 at 07:17
Matthew Peters
I tried the habit stacking thing with my dad. Took his pill right after he brushed his teeth. He forgot to brush for three days. So now he takes it after his morning coffee. Simple. Works. Also, I bought him a little alarm clock that just says ‘PILLS’ in big letters. He loves it.
December 2, 2025 at 11:33
Write a comment