Most people with fatty liver don’t feel sick. No pain. No warning. Just a routine blood test that says ALT is high. Then comes the ultrasound: ‘You have fat in your liver.’ But what does that really mean? Is it just a harmless buildup of fat, or is it something more dangerous? The difference between NAFLD and NASH isn’t just medical jargon-it’s the line between a condition you can reverse and one that could lead to cirrhosis, liver failure, or even cancer.
What Exactly Is NAFLD?
NAFLD stands for Non-Alcoholic Fatty Liver Disease. It’s not caused by drinking alcohol. It’s caused by too much fat building up in liver cells-usually because of insulin resistance, obesity, or metabolic syndrome. The American Association of Family Physicians defines it simply: 5% or more of your liver is fat, with no signs of damage or inflammation. This version is called NAFL-simple fatty liver. It’s the most common form, affecting about 80% of people diagnosed with NAFLD.
Here’s the good news: if you’re in this group, your liver isn’t actively being damaged. Studies show that over 15 years, only about 12% of people with NAFL develop serious fibrosis. Most stay stable. Some even improve with weight loss or better blood sugar control. But here’s the catch: you don’t know if you’re in this low-risk group unless you get tested properly. Many assume ‘fatty liver’ means they’re fine. They’re not.
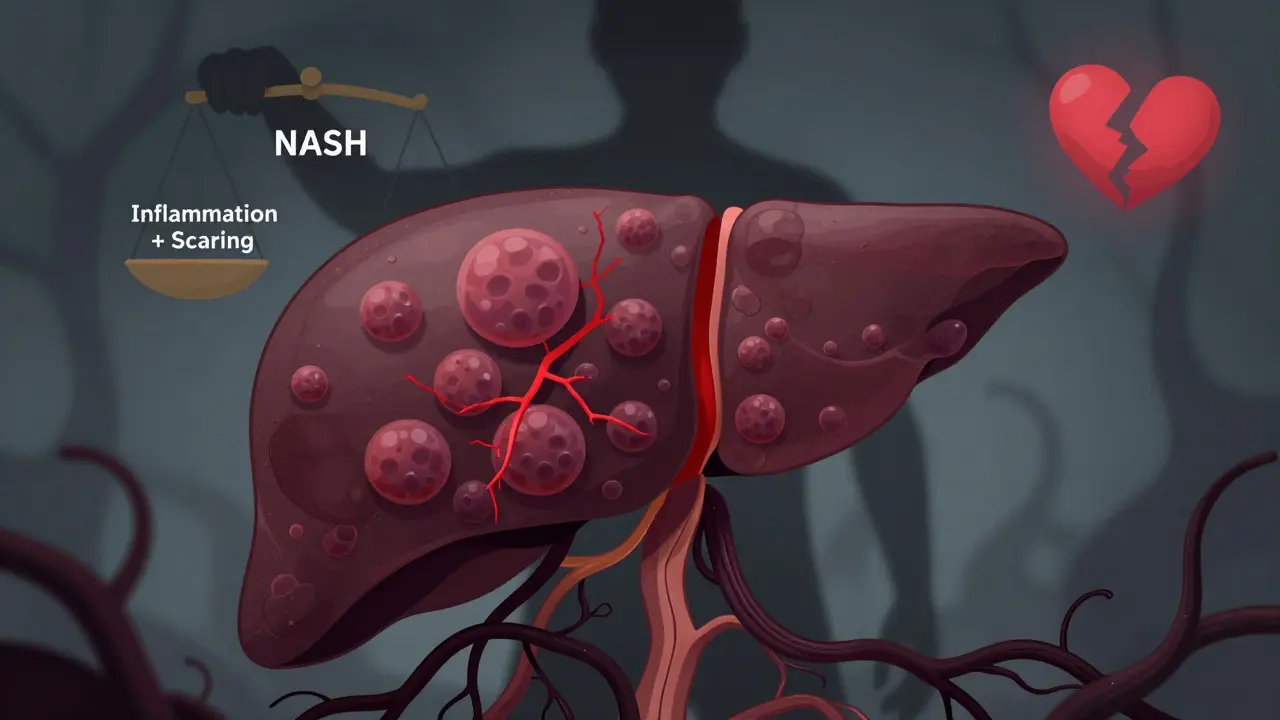
When NAFLD Turns Into NASH
NASH-Non-Alcoholic Steatohepatitis-is the dangerous cousin of NAFL. It’s not just fat anymore. Now your liver cells are swollen, inflamed, and dying. This is called hepatocyte ballooning. And it triggers scarring-fibrosis. The difference isn’t subtle. It’s the difference between a car with a dirty engine and a car with a cracked cylinder head.
NASH happens in about 20% of people with NAFLD. That’s 1 in 5. And once it starts, the damage doesn’t stop on its own. The American Liver Foundation reports that 20-40% of NASH patients develop cirrhosis within 10 to 20 years. That’s irreversible scarring. Your liver can’t regenerate properly at that point. And once cirrhosis sets in, your risk of liver cancer jumps dramatically.
What pushes someone from NAFL to NASH? It’s not random. The biggest risk factors are all tied to metabolism: obesity (70-90% of NASH patients), type 2 diabetes (50-70%), high blood pressure (60-75%), and sleep apnea (30-50%). If you have three or more of these, you’re in the high-risk zone. The 2023 guidelines from AASLD and EASL now call this group MASLD-Metabolic Dysfunction-Associated Steatotic Liver Disease. The name change isn’t just politics. It’s recognition: this isn’t about alcohol. It’s about how your body handles sugar and fat.
Fibrosis: The Silent Progression
Fibrosis is the real threat. Not the fat. Not even the inflammation. It’s the scar tissue. Think of your liver like a sponge. When it’s healthy, it bounces back. When it’s scarred, it stiffens. And once it turns into a rubber brick, it can’t filter toxins, make proteins, or store energy like it should.
Fibrosis is staged from 0 to 4:
- Stage 0: No scarring
- Stage 1: Minor scarring around veins
- Stage 2: Scarring spreading
- Stage 3: Bridging fibrosis-scars start connecting
- Stage 4: Cirrhosis-your liver is mostly scar tissue
Here’s what matters: if you’re at stage 3 or 4, your 10-year risk of dying from liver disease is 12-25%. If you’re at stage 0-2, it’s less than 2%. That’s a 10-fold difference. And the scary part? Most people don’t know their stage until it’s too late. Symptoms? Fatigue, vague belly discomfort, unexplained weight loss. But 68% of people with fatty liver have zero symptoms when diagnosed.
How Do You Know If You Have NASH?
There’s no single blood test for NASH. ALT and AST levels might be elevated, but not always. Some people with NASH have normal liver enzymes. Ultrasound can show fat-but it misses early inflammation. MRI-PDFF is better for measuring fat, but still can’t confirm scarring or ballooning.
The only way to definitively diagnose NASH is a liver biopsy. It’s invasive. It carries a tiny risk of bleeding. But it’s the only test that can show you the real picture: fat + inflammation + ballooning = NASH. The British Liver Trust says biopsy should only be done when there’s high suspicion of advanced fibrosis. Why? Because most people with simple fatty liver don’t need it.
So doctors use non-invasive tools first:
- FIB-4 score: Uses your age, ALT, AST, and platelet count. Above 1.30? Possible fibrosis. Above 2.67? High chance of advanced fibrosis.
- APRI score: Based on AST and platelets. Above 0.5? Watch out.
- FibroScan: Measures liver stiffness. Over 7.1 kPa? Likely significant fibrosis. Over 10 kPa? Strongly suggests stage 3 or 4.
If these tests point to advanced fibrosis, a biopsy is recommended. But even FibroScan isn’t perfect. Liver tissue is uneven. A biopsy might miss the scarred area. That’s why doctors look at the whole picture-your weight, blood sugar, cholesterol, and test results together.
What Happens If You Do Nothing?
Let’s say you’re diagnosed with NAFL. You’re told to lose weight. You say, ‘I’ll get to it.’ Then you forget. Two years later, your ALT is higher. Your FibroScan shows 8.5 kPa. You get a biopsy. It’s NASH. Stage 2 fibrosis.
That’s the timeline for many people. Progression isn’t fast. But it’s relentless. The 2019 Hepatology study showed 41.7% of NASH patients developed significant fibrosis over 15 years. Only 12.3% of NAFL patients did. That’s a 3.5x higher risk.
And it’s not just your liver. Cardiovascular disease kills more people with NAFLD than liver disease does. 42% of deaths in NAFLD patients are from heart attacks or strokes. Your liver is a mirror. If it’s fatty, your arteries are probably clogged too.

Can You Reverse It?
Yes. But only if you act early.
Weight loss is the most proven treatment. Losing 7-10% of your body weight can reverse NASH back to simple fatty liver in 90% of cases. It can also reduce fibrosis by 85%. That’s not a guess. That’s from the 2023 International NASH Registry. One patient on a patient forum wrote: ‘Lost 10% in 18 months. My biopsy showed no NASH anymore.’
Exercise helps-even without weight loss. Just 150 minutes a week of brisk walking improves liver fat and insulin sensitivity. Cutting sugar and refined carbs matters more than counting calories. Soda, white bread, pastries-they feed the fat in your liver.
Medications? Until recently, there were none. But in March 2023, the FDA approved resmetirom (Rezdiffra) for people with moderate to advanced fibrosis. It’s the first drug proven to reduce liver fat and fibrosis in NASH patients. It’s not a cure. It’s a tool-for those who’ve already progressed.
For most people, though, the answer is still lifestyle. No magic pills. No shortcuts. Just food, movement, and consistency.
Who Should Be Screened?
You don’t need to be sick to be at risk. If you have:
- BMI over 28
- Type 2 diabetes
- High blood pressure
- High triglycerides or low HDL
- Waist size over 40 inches (men) or 35 inches (women)
Then you should get tested. Start with a simple blood test: ALT and AST. If they’re high, ask for a FibroScan or FIB-4 calculation. Don’t wait for symptoms. They won’t come until it’s too late.
Primary care doctors are screening more now. But only 32% feel confident managing advanced cases. If your doctor says, ‘Just lose weight,’ and doesn’t follow up with fibrosis tests, ask for a referral to a hepatologist. You’re not overreacting. You’re protecting your future.
The Big Picture
By 2030, over a third of the world’s population could have MASLD. NASH-related liver transplants in the U.S. will double. The economic cost? Over $100 billion a year in the U.S. alone.
This isn’t a rare disease. It’s a silent epidemic. And the worst part? It’s preventable. Most people don’t know they’re at risk until their liver is half scar tissue. But if you catch it early-before fibrosis-you have power. You can turn it around. Not with a pill. Not with a miracle. With your plate, your steps, your choices.
The liver is one of the few organs that can heal itself. But only if you give it a chance.
Is NAFLD the same as NASH?
No. NAFLD is the umbrella term for all fatty liver cases not caused by alcohol. It includes two types: NAFL (simple fat buildup with no damage) and NASH (fat plus inflammation and liver cell injury). NASH is the more serious form that can lead to scarring and cirrhosis.
Can you have NASH without being overweight?
Yes. While most people with NASH are overweight or have type 2 diabetes, about 10-20% are of normal weight. This is sometimes called ‘lean NASH.’ It’s linked to insulin resistance, genetics, or gut health issues. Don’t assume you’re safe just because you’re thin.
Does fatty liver always lead to cirrhosis?
No. Only about 20-40% of NASH patients develop cirrhosis over 10-20 years. Most people with simple fatty liver (NAFL) never progress to serious damage. The key is early detection and lifestyle change. Progression isn’t guaranteed-it’s preventable.
What’s the difference between MASLD and NAFLD?
MASLD (Metabolic Dysfunction-Associated Steatotic Liver Disease) is the new name for NAFLD, adopted in 2023. It replaces the outdated ‘non-alcoholic’ label with a focus on metabolic health-like insulin resistance, obesity, and high blood sugar. The change helps reduce stigma and better reflects the real cause: how your body processes sugar and fat.
Are there any drugs to treat NASH?
Yes. In March 2023, the FDA approved resmetirom (Rezdiffra) for adults with NASH and moderate to advanced fibrosis. It’s the first drug proven to reduce liver fat and fibrosis. But it’s not for everyone. Lifestyle changes remain the first-line treatment for most people. Other drugs are still in clinical trials.
How do I know if my fatty liver is getting worse?
You won’t feel it. That’s the danger. The only way to know is through testing: FIB-4 score, FibroScan, or liver biopsy. If your ALT stays high over time, or your FibroScan reading climbs above 7.1 kPa, it’s time to see a specialist. Don’t wait for symptoms like fatigue or belly pain-they appear late.

Comments
Annie Choi
NAFLD to NASH is the silent killer no one talks about until it's too late. I had a friend go from 'oh it's just fat' to transplant list in 3 years. No symptoms. No warning. Just a FibroScan that said 11.2 kPa and a biopsy that confirmed stage 4. You think you're fine because you're not jaundiced or vomiting. You're wrong. Get tested. Now.
January 15, 2026 at 02:17
Iona Jane
They don't want you to know the truth. Big Pharma and the sugar industry funded the 'just lose weight' narrative so you keep buying their meds and their snacks. FibroScan is expensive. Biopsy is invasive. But what's cheaper? Dying at 45 or paying $800k for a liver? They're letting you rot so they can sell you the cure later.
January 16, 2026 at 06:19
Jaspreet Kaur Chana
In India we call this 'jhatka liver' - the silent killer that sneaks up because everyone thinks if you're not drunk or yellow, you're fine. My uncle, 52, normal weight, no diabetes, just high triglycerides - got diagnosed with NASH stage 3. They said it was 'lean NASH'. Turns out his dad had it too. Genetics. Stress. Roti and ghee every day. We thought it was just 'Indian metabolism'. No. It's metabolic dysfunction. MASLD. Call it what it is. And yes, 150 minutes of walking a week? That's real. I did it. Lost 9%. FibroScan dropped from 9.8 to 5.3. No drug. Just sweat.
January 17, 2026 at 20:36
Haley Graves
If your doctor says 'lose weight' and doesn't order a FIB-4 or FibroScan, find a new doctor. That's like saying 'your cholesterol is high, just eat less' and not checking for plaque. You're not being dramatic. You're being responsible. The liver doesn't scream until it's broken. Don't wait for the scream.
January 19, 2026 at 05:22
ellen adamina
I had a normal ALT but a FibroScan of 8.1. Biopsy confirmed NASH stage 2. I was shocked. I exercise. I don't drink. I eat salad. Turns out my 'healthy' smoothies were just sugar water. Fructose is the real villain. Not fat. Not carbs. Fructose. It's metabolized in the liver like alcohol. That's why even thin people get it. I cut all juice, soda, and 'natural' sweeteners. 14 months later, no NASH. Just NAFL. And I didn't even lose 10%.
January 20, 2026 at 19:52
Tom Doan
How convenient. The medical establishment rebrands NAFLD as MASLD - now we can blame metabolism instead of poor lifestyle choices. And suddenly, the FDA approves a $100,000-a-year drug for stage 3 fibrosis. But let's not mention that the only proven treatment remains: stop eating processed food and move your body. The new name doesn't change the cause. It just makes the pharmaceutical pipeline look more sophisticated.
January 20, 2026 at 22:01
Nishant Garg
My cousin in Delhi, 48, thin, vegetarian, no alcohol - got NASH. He ate too much white rice, too much ghee in dal, too much mango lassi. He thought 'vegetarian' meant 'healthy'. No. It meant 'carb-loaded with saturated fat'. He started walking 45 minutes every morning. Cut rice. Swapped ghee for olive oil. Lost 8%. Biopsy showed fibrosis regressed. No magic. Just science. And yes, it's possible even if you're not obese. Don't assume your diet is clean. It might be poison.
January 21, 2026 at 03:29
Nilesh Khedekar
Listen, I'm not here to coddle you. You think your 'occasional' soda is fine? Your 'healthy' granola bar is loaded with HFCS? Your 'light' yogurt has 18g of sugar? You're feeding your liver poison and calling it a lifestyle. You're not 'busy'. You're lazy. And your liver doesn't care how hard you work. It just dies. Slowly. Quietly. And then you're dead. Get a FibroScan. Now. Before you're one of those statistics.
January 21, 2026 at 08:19
Jami Reynolds
There's a 92% correlation between MASLD and glyphosate exposure. The EPA has known since 2018. The FDA hasn't. Why? Because the same corporations that make Roundup also own the pharmaceutical companies selling resmetirom. The real epidemic isn't metabolic dysfunction. It's corporate poisoning. You're being chemically castrated by your food supply. Your liver is a bioindicator. It's screaming. But the system is deaf.
January 22, 2026 at 19:46
Amy Ehinger
I didn't even know I had fatty liver until my insurance sent me a letter saying 'high ALT detected, consider screening'. I thought it was a typo. Turned out I was stage 2 NASH. I was 32. I didn't feel sick. I didn't look sick. But my liver was screaming. I started walking with my dog. Cut out the midnight ice cream. Stopped drinking kombucha because it had 12g sugar. Didn't even need to lose weight. Just changed the kind of food I ate. Now my FibroScan is 4.9. I'm not a hero. I just listened. And you can too.
January 22, 2026 at 22:57
Niki Van den Bossche
The entire concept of 'fatty liver' is a construct of late-stage capitalism. We've been conditioned to view the body as a machine that can be optimized, commodified, and monetized - hence the rise of FibroScan as a profit center, the rebranding of NAFLD as MASLD to unlock new drug patents, and the cult of 'lifestyle intervention' that absolves systemic failure. Your liver isn't broken. The system is. And until we dismantle the metabolic industrial complex, no amount of walking or kale will heal the wound we've been taught to ignore.
January 24, 2026 at 10:35
Jan Hess
Just wanted to say thanks for this post. I got diagnosed last year with NAFL. Thought I was fine. Then I read this. Did the FIB-4. Score was 1.8. Got a FibroScan. 7.8. That's when I panicked. Started walking. Stopped soda. Cut out white bread. Lost 7% in 5 months. Re-tested. FibroScan down to 5.1. No NASH anymore. It's not glamorous. No pills. No magic. Just showing up. Every day. You can do this.
January 24, 2026 at 18:50
Diane Hendriks
Let me be perfectly clear: if you have a BMI over 28 and are over 40, and you haven't had a FibroScan or FIB-4 test, you are medically negligent. Your ignorance is not innocence. It is a choice - a choice to risk cirrhosis, liver cancer, and death. This is not a suggestion. It is a public health imperative. The data is unequivocal. The time for passive observation is over. Get tested. Now.
January 24, 2026 at 22:10
Write a comment