A rare tumor in your adrenal gland can send your blood pressure skyrocketing for no reason at all. You might feel like you're having a panic attack-sweating buckets, heart racing, head pounding-but no anxiety medication helps. That’s because it’s not anxiety. It’s pheochromocytoma, a tumor that tricks your body into flooding your system with adrenaline. And if you don’t know what you’re dealing with, you could end up in the ER with a blood pressure of 240/130-or worse.
What Exactly Is a Pheochromocytoma?
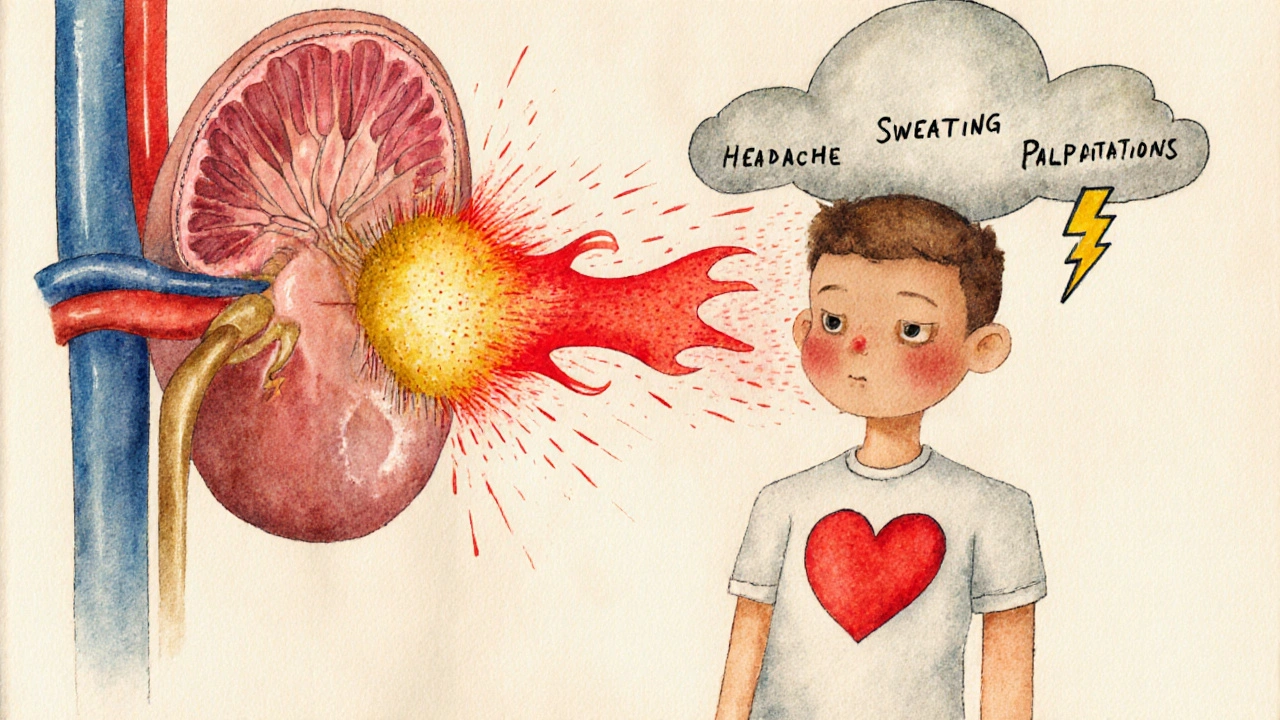
Pheochromocytoma is a tumor that grows in the middle part of the adrenal gland, called the medulla. These glands sit on top of your kidneys and normally make small amounts of adrenaline and noradrenaline to help you respond to stress. But when a pheochromocytoma forms, it starts pumping out way too much of these hormones-on its own, even when you’re sitting still.
It’s not cancer in most cases. About 90% of these tumors are benign. But that doesn’t mean they’re harmless. The hormones they release cause sudden, violent spikes in blood pressure. These episodes can last minutes or hours, and they often come without warning. Some people get them when they exercise, get scared, or even when they pee-if the tumor is in the bladder wall (called a paraganglioma).
It’s rare. Only about 1 in 1,000 people with high blood pressure have this tumor. But because it’s so uncommon, most doctors don’t see it often. The average person waits over three years before getting the right diagnosis. Many are told they have anxiety, migraines, or panic disorder. That’s because the symptoms look exactly like them.
The Classic Triad: Headache, Sweating, Palpitations
If you’ve ever had a sudden episode where your heart felt like it was going to burst, your head throbbed like a drum, and you were drenched in sweat-even in a cool room-you might have experienced a pheochromocytoma spell.
These three symptoms happen together in most cases:
- Severe headaches (85-90% of patients)
- Profuse sweating (75-80%)
- Palpitations or racing heart (70-75%)
Other signs include:
- Blood pressure spikes above 180 mmHg systolic
- Pale or ashen skin
- Abdominal pain or nausea
- Unexplained weight loss
- Feelings of doom or panic
What makes this different from regular high blood pressure? Essential hypertension doesn’t come in waves. It’s steady. Your blood pressure is just always high. With pheochromocytoma, it’s like someone flips a switch. You go from normal to emergency in seconds. Then, just as suddenly, it drops-sometimes even too low, causing dizziness when you stand up.
Why Is It So Hard to Diagnose?
Most primary care doctors will see maybe one or two cases in their entire career. So when a patient walks in with high blood pressure and anxiety-like symptoms, the default assumption is stress or mental health.
But there’s a test that catches this every time: measuring metanephrines. These are breakdown products of adrenaline and noradrenaline. When the tumor is active, these chemicals flood your blood and urine.
The gold standard is a 24-hour urine test for fractionated metanephrines. It’s 96-99% sensitive. Blood tests for plasma-free metanephrines are almost as good. If your levels are more than three times the upper limit of normal, you almost certainly have a pheochromocytoma.
But here’s the catch: some people have borderline results. That’s where things get messy. About 15-20% of people with slightly elevated levels don’t actually have a tumor. They’re told they might have one, get unnecessary scans, and live in fear. That’s why doctors don’t jump to imaging right away. First, you need solid biochemical proof.
Imaging: Finding the Tumor
Once the blood or urine test confirms the diagnosis, the next step is imaging. The old rule was the “10-10-10 rule”: 10% of tumors are in both adrenal glands, 10% are outside the adrenal gland (paragangliomas), and 10% are cancerous.
But newer data shows that’s outdated. In people with inherited gene mutations-like SDHB, VHL, or RET-the chance of multiple tumors or extra-adrenal tumors is much higher. That’s why genetic testing is now recommended for everyone diagnosed with pheochromocytoma, not just those with a family history.
CT or MRI scans find the tumor in most cases. But the newest tool is 68Ga-DOTATATE PET/CT. It’s more accurate than traditional scans, especially for small or extra-adrenal tumors. It’s not available everywhere yet, but in major centers, it’s becoming the go-to for staging.
Surgery: The Only Cure
Here’s the good news: if the tumor is caught early, surgery can cure you. In 85-90% of cases, blood pressure returns to normal after the tumor is removed. People who were on three or four blood pressure medications wake up after surgery and are off them within weeks.
But surgery isn’t simple. You can’t just go in and yank out the tumor. The tumor is basically a time bomb of adrenaline. If you touch it without preparing the body, the surge of hormones can cause a deadly hypertensive crisis.
That’s why pre-op preparation is non-negotiable.
For 7-14 days before surgery, patients take phenoxybenzamine, a drug that blocks adrenaline receptors. This stops the blood vessels from clamping down. Doctors also push patients to drink 2-3 liters of water a day and eat a high-sodium diet. Why? Because the tumor causes chronic blood vessel constriction, which shrinks your blood volume by 20-30%. You’re basically dehydrated in disguise. Replenishing fluids prevents dangerous drops in blood pressure during surgery.
The surgery itself is usually done laparoscopically-small incisions, camera, instruments. At high-volume centers, it’s successful in 95% of cases with under 2% major complications. But if the tumor is huge, stuck to nearby organs, or bleeding heavily, the surgeon may need to switch to open surgery. That’s rare, but it happens in 5-8% of cases.
What Happens After Surgery?
Recovery is quick for most. You’re usually out of the hospital in 1-2 days. Most people are back to work in two weeks.
But there are two big catches.
First, if you had a tumor on both adrenal glands-or if both had to be removed-you can’t make cortisol or aldosterone anymore. You’ll need lifelong steroid replacement: hydrocortisone and fludrocortisone. One patient described it as “a daily pill routine that reminds you you’re still not normal.”
Second, even if you’re cured, you need follow-up. About 12% of people report chronic fatigue for six months or longer after surgery. No one knows why. It’s not the steroids. It’s not the surgery. It just happens. And for those with SDHB mutations, there’s a 30-50% lifetime risk of developing another tumor-sometimes cancerous. They need yearly whole-body MRIs for life.

Genetic Testing Isn’t Optional
Thirty-five to forty percent of pheochromocytomas are tied to inherited gene mutations. That means if you have one, your siblings, children, or parents might have it too-and not even know it.
Genes like SDHB are especially dangerous. They’re linked to higher cancer risk and tumors in unusual places. If you test positive for SDHB, your doctor will want to scan your neck, chest, and abdomen regularly. Other genes like RET (linked to multiple endocrine neoplasia) or VHL (von Hippel-Lindau syndrome) mean you’re at risk for other tumors too-like kidney cancer or brain tumors.
That’s why genetic testing is now standard. It’s not just about you. It’s about your family.
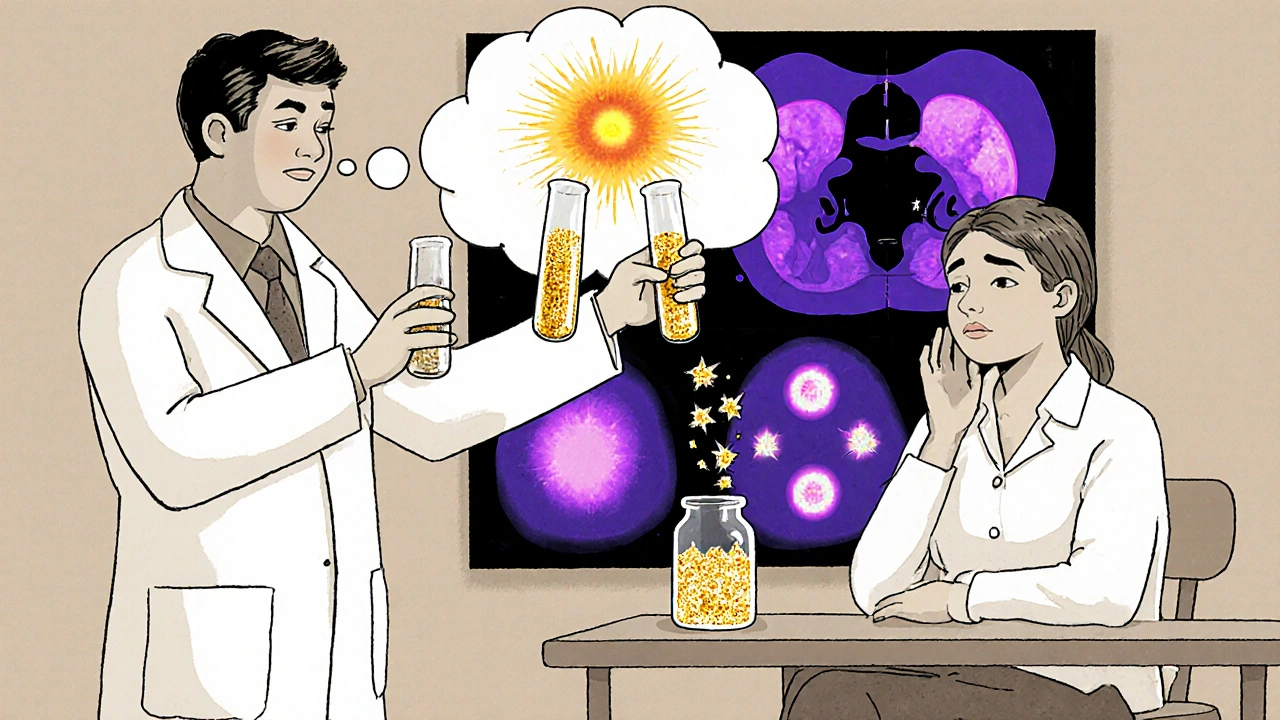
What About the Future?
For the small number of people with metastatic pheochromocytoma, things are changing fast. New treatments like 177Lu-DOTATATE (a type of radiation therapy) are helping. In early trials, 65% of patients saw their tumors shrink or stop growing.
There’s also a new drug called Belzutifan, approved for VHL-related tumors. It blocks a protein called HIF-2α that tumors use to grow. Early results show it can shrink adrenal tumors without surgery.
And researchers are working on blood tests that can detect tumor DNA before the tumor even shows up on a scan. That could mean catching it years earlier.
Bottom Line: Don’t Ignore the Spells
If you’ve had episodes of extreme sweating, pounding headaches, and heart racing-with no clear trigger-don’t brush it off. Ask your doctor about metanephrines. It’s a simple blood or urine test. No needles, no fasting, no big hassle.
Most people with pheochromocytoma live normal lives after surgery. But if you don’t get diagnosed, the risks are real: stroke, heart attack, or sudden death during surgery for something else-like gallbladder removal-because the tumor wasn’t known.
It’s rare. But it’s treatable. And if you’re the one who’s been told you’re just anxious for years? You might not be. You might just have a tiny tumor in your adrenal gland that’s been screaming for attention.

Comments
shubham seth
Yo, this is wild-pheochromocytoma is basically your adrenal gland going full Tony Montana at 3 a.m. while you’re trying to nap. I’ve seen patients with BP 220/140, sweating like they just ran a marathon in a sauna, and all they got was Xanax and a pity nod. Meanwhile, the tumor’s just chilling there, pumping adrenaline like it’s running a crypto mining rig. If your doc doesn’t check metanephrines after three ‘panic attacks,’ they’re not a doctor-they’re a glorified Google autocomplete.
November 18, 2025 at 13:50
Leslie Douglas-Churchwell
Let’s be real: this isn’t medicine-it’s corporate obfuscation. The pharmaceutical industry doesn’t want you to know that a $50 urine test can cure what they’ve been selling as ‘anxiety’ for decades. Benzodiazepines? SSRIs? Please. Those are just Band-Aids on a nuclear reactor. And don’t get me started on how Big Pharma funds ‘guidelines’ that bury the metanephrine protocol. 🤫💎 #WakeUpSheeple #AdrenalTruth
November 20, 2025 at 01:01
Gordon Mcdonough
Man I’ve had this for years and no one believed me I told my PCP I was having these episodes and he said I was just stressed out and to try yoga I’m like bro I’m not meditating I’m having a hypertensive crisis and then one day I passed out in Target and they did the test and boom tumor 1.8cm left adrenal and now I’m off all meds and I just wanna scream at every doctor who told me I was crazy
November 21, 2025 at 03:24
Jessica Healey
OMG I’m literally crying right now. I thought I had severe anxiety for 7 years. I’d get these attacks after coffee, or walking up stairs, or even just thinking about taxes. I had panic disorder diagnoses, therapy, meds-I even did a ketamine retreat. Turns out my adrenal gland was just… throwing a rave. Surgery was a breeze. I haven’t felt this calm since high school. 🤍
November 21, 2025 at 07:36
Levi Hobbs
Great breakdown. I’m a PA and we see this maybe once every 3 years, but when we do, it’s life-changing. The key is recognizing the episodic nature-essential HTN is constant. Also, the pre-op fluid loading is critical. I’ve seen cases where they skipped it and the patient coded on the table. Always check metanephrines if there’s any suspicion. Simple test. Huge payoff.
November 22, 2025 at 15:51
henry mariono
Thanks for writing this. I’ve been waiting for someone to explain this clearly. I was diagnosed last year after a 5-year diagnostic odyssey. I didn’t know what to believe anymore. Now I’m off meds, sleeping through the night, and actually enjoying coffee again. It’s weird to feel normal.
November 24, 2025 at 12:45
Sridhar Suvarna
This is why we need more awareness in primary care. In India, we rarely test for metanephrines unless the patient is literally screaming on the table. Many cases get labeled as psychosomatic. But this condition is real. And treatable. And if we catch it early, we save lives. Let’s push for screening in high-risk groups. No more guessing.
November 26, 2025 at 12:28
Joseph Peel
There’s a quiet tragedy here: patients who spend years being dismissed as ‘hypochondriacs’ or ‘overreactive.’ The medical system often pathologizes symptoms it doesn’t understand. This isn’t just about a tumor-it’s about listening. The triad is unmistakable if you know to look. The science is solid. The solution exists. Why isn’t this in every med school curriculum?
November 26, 2025 at 15:58
Kelsey Robertson
Ugh. Of course it’s a tumor. Everything is a tumor if you look hard enough. First they tell you it’s anxiety, then they tell you it’s a tumor, now they’re telling you to get genetic tested because your cousin’s dog might have had a similar mutation. I’m supposed to believe that 40% of these are genetic? That’s just fear-mongering dressed up as science. Next they’ll say your childhood trauma caused the tumor. Please.
November 27, 2025 at 15:49
Joseph Townsend
I had one. And let me tell you-it wasn’t just a tumor. It was a cosmic prank. One minute I’m fine, next minute I’m convinced the world is ending, my heart’s trying to escape my chest, and I’m drenched like I just swam in a hurricane. I thought I was dying. I called 911 three times. And the ER docs? They looked at me like I was a weirdo who drank too much Red Bull. Then the test came back. And the surgeon? He said, ‘You’re lucky you’re still alive.’ I cried in the waiting room. Not from fear-from relief. I didn’t know I was sick. I thought I was broken.
November 29, 2025 at 09:50
Bill Machi
This is why America’s healthcare is failing. You have to be near death before someone considers a rare disease. I had this for 4 years. I went to 7 doctors. 5 of them prescribed antidepressants. One told me to stop eating carbs. The last one? He ran the metanephrine test because his wife had the same thing. That’s not medicine. That’s luck. And now I’m paying $20k for surgery because my insurance said it was ‘not medically necessary’ until I had a stroke scare. This system is a joke.
November 30, 2025 at 00:48
Elia DOnald Maluleke
In the grand tapestry of human physiology, the adrenal medulla is a silent sentinel-its hormonal whispers often drowned by the cacophony of modern diagnostics. Yet, when it screams, it does so with the ferocity of a supernova. This condition is not merely a tumor; it is a metaphysical disturbance-a rebellion of the endocrine self against the illusion of normalcy. To dismiss it as anxiety is to mistake the storm for the sky. The cure is surgical, yes-but the awakening? That is spiritual. We must not only treat the gland. We must listen to the soul that has been screaming through it.
November 30, 2025 at 09:57
Write a comment