Antibiotic Therapy: What You Need to Know
Antibiotics save lives, but they work only for bacterial infections. If you take them the wrong way, they won’t help and can cause harm — from side effects to drug resistance. This page collects clear, useful advice so you can use antibiotics safely and get better faster.
How antibiotics work and how they’re chosen
Antibiotics either kill bacteria or stop them from growing. Doctors pick a drug based on where the infection is (throat, lungs, sinuses, urine), likely bacteria, and test results when available. For example, ampicillin might be used for certain sinus or ear infections, while other cases need a different class like macrolides or cephalosporins.
If your doctor orders a culture, stick with the prescribed antibiotic until you get results unless told otherwise. That test helps switch to the narrowest, most effective drug — which lowers side effects and reduces resistance.
Using antibiotics safely: dosing, side effects, and resistance
Follow the prescription exactly: dose, timing, and full course length matter. Stopping early because you feel better can leave surviving bacteria that come back stronger. Missing doses reduces drug levels and lowers the chance of clearing the infection.
Watch for common side effects: nausea, diarrhea, or rash. Severe allergic reactions are rare but require immediate care. If you take blood thinners like warfarin (Coumadin), many antibiotics change how those drugs work — get your INR checked or talk to your prescriber before starting a new antibiotic.
Drug interactions matter. For instance, some antibiotics interact with antacids, birth control, or statins. Tell your clinician all medicines and supplements you use. If you’re pregnant, breastfeeding, or have liver or kidney issues, the safest antibiotic choice can change.
Antibiotic resistance happens when bacteria survive and adapt. Avoid pressure to get antibiotics for viral illnesses like colds or most sore throats. Use the right drug, at the right dose, for the right time. Handwashing, vaccines, and good wound care reduce the need for antibiotics in the first place.
If symptoms don’t improve in 48–72 hours, call your doctor. Worsening fever, breathing trouble, severe pain, or signs of an allergic reaction mean seek immediate care. Safely dispose of unused pills — don’t keep partial courses “just in case.” Many pharmacies offer take-back programs.
Want real-world examples? Read a patient diary about ampicillin for sinus infection, or our guides on interactions with blood thinners and safe buying tips. Use these resources to ask better questions at your next visit and to manage antibiotics responsibly.
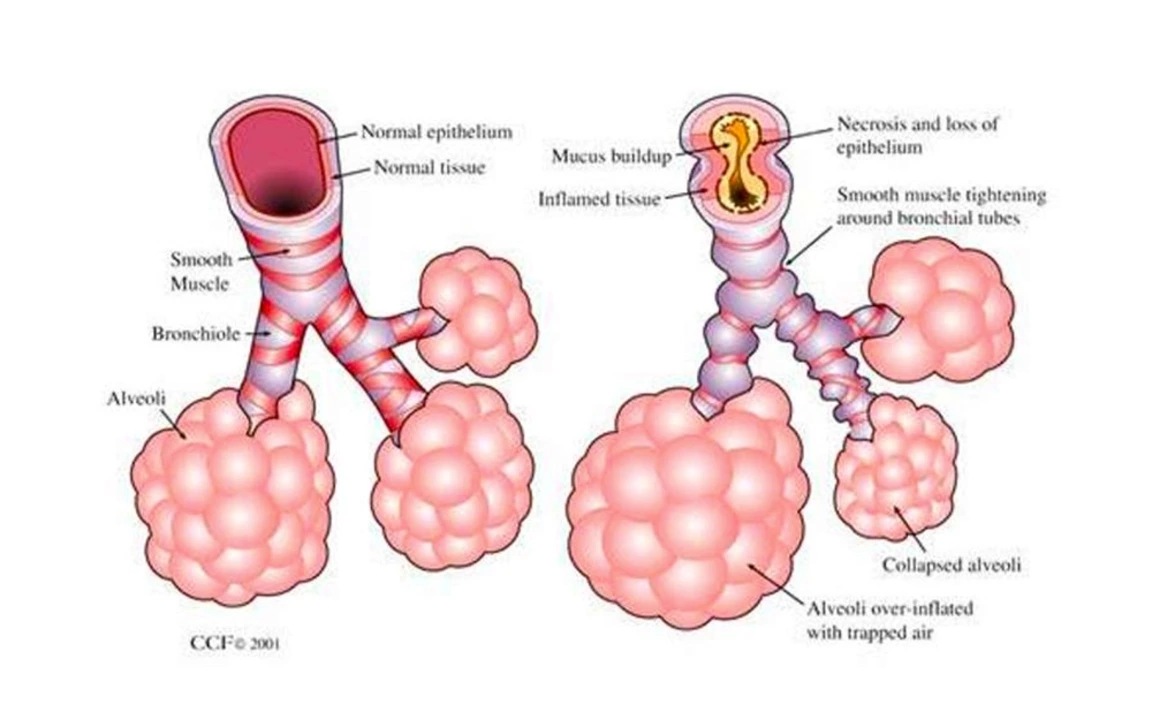
As a blogger, I recently came across some fascinating information about the use of azithromycin in treating bronchiolitis. Azithromycin is an antibiotic that has shown promising results in reducing the severity of bronchiolitis symptoms, which primarily affects infants and young children. It works by fighting the bacteria that cause the infection, helping to alleviate the inflammation in the airways. Studies are still ongoing, but early findings suggest that azithromycin may be a valuable addition to the current treatment options for bronchiolitis. I am eager to follow the progress of this research and share updates with my readers in the future.