Motor Function: Causes, Simple Tests and How to Improve Movement
Noticing slowness, clumsiness, or weakness? Those are changes in motor function — how your brain, nerves and muscles work together to move. You don’t need medical training to spot when something’s off, and there are straightforward steps you can take right away to protect your mobility.
What commonly affects motor function
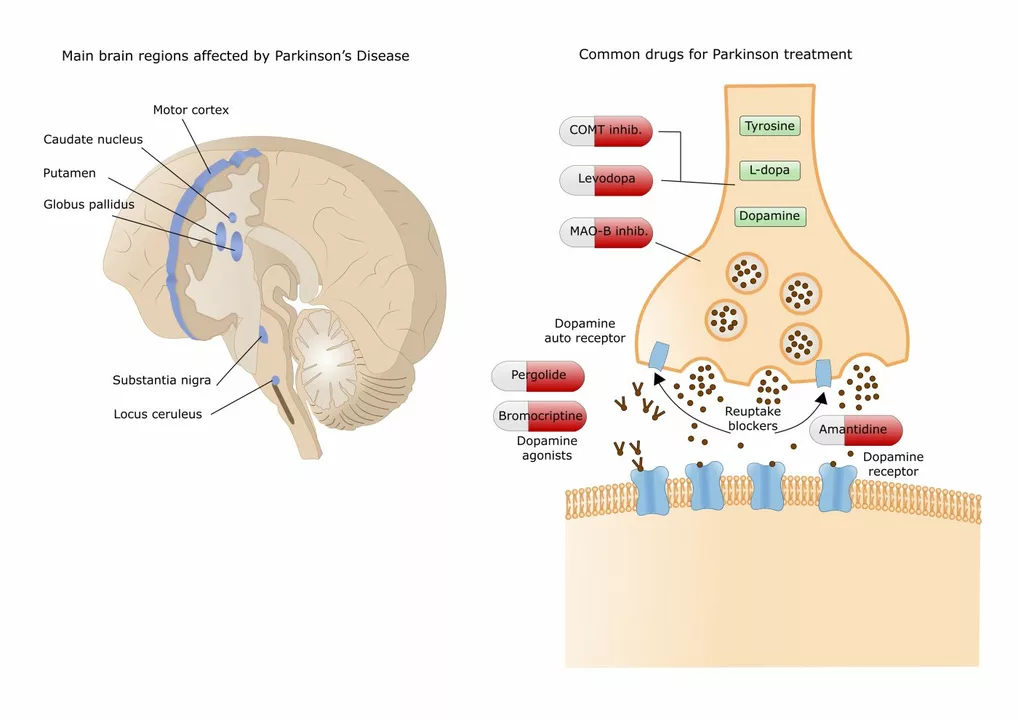
Think of motor problems as coming from three places: the brain/spinal cord (stroke, Parkinson’s, multiple sclerosis), the nerves (peripheral neuropathy, diabetes), and the muscles or joints (arthritis, injury). Medications, infections, low electrolytes and poor nutrition can also slow you down. Age doesn’t mean you must lose movement — it just raises the chance of certain problems.
Symptoms you’ll notice: sudden weakness on one side, trouble walking, shaky or slow movements, loss of coordination, frequent stumbling, or tasks that used to be easy feeling hard. If speech or balance changes suddenly, treat it as an emergency.
Quick checks you can do at home
Want to know if you should see a doctor? Try these simple tests: walk a few steps and watch for a limp or uneven stride; stand with feet together and eyes closed for 20 seconds (Romberg test) to check balance; touch your nose then a partner’s finger repeatedly to test coordination; squeeze fingers to test hand strength. These aren’t diagnostic, but they help you describe the problem clearly to a clinician.
If weakness is sudden, severe, or paired with facial droop or trouble speaking, call emergency services. For gradual issues, book a visit with your GP or neurologist for a full exam and possibly imaging or nerve tests.
Treatments focus on the cause. Stroke, infections, or medication side effects need prompt medical care. Chronic conditions often improve with a mix of therapy, medicines, and lifestyle changes. Physical and occupational therapy are central — they teach movement strategies, strength exercises and safe ways to do daily tasks.
Simple home exercises help: seated leg lifts, heel raises, toe walks, short balance stands while holding a chair, and gentle arm lifts. Start slow, repeat daily, and stop if you feel sharp pain. A therapist can tailor progressions and show safe forms.
Other practical steps: review your medicines with a pharmacist (some drugs cause dizziness or weakness), manage blood sugar and blood pressure, keep Vitamin D and B12 levels checked, wear sensible shoes, and remove trip hazards at home. Small changes cut fall risk and improve confidence.
If you’re rebuilding after illness, set real goals: walk to the mailbox, climb one flight of stairs, or stand from a chair without using hands. Celebrate small wins — they add up.
Curious for deeper reads? Check our articles on joint conditions, migraine treatments that affect movement, and rehab strategies. If you want, tell us what symptoms you’ve noticed and we’ll point you to the most relevant guides.
As a blogger, I recently came across an intriguing topic - the potential of Trihexyphenidyl and music therapy in improving motor function for those suffering from Parkinson's disease. Trihexyphenidyl, an anticholinergic medication, has shown promise in alleviating motor symptoms in Parkinson's patients, while music therapy has been known to help with movement and coordination. Combining these two approaches could potentially offer a more effective treatment option for patients dealing with this debilitating condition. I am eager to explore this topic further and share my findings with my readers, as it could provide hope for those struggling with Parkinson's disease and their loved ones. Stay tuned for my in-depth analysis on the effectiveness of Trihexyphenidyl and music therapy in enhancing motor function in Parkinson's patients.