When you have a sore knee, a stiff shoulder, or aching muscles, you have choices. You can reach for a pill you swallow, or you can rub on a gel or cream. Both aim to relieve pain, but they work in very different ways-and the difference matters more than you think.
How Your Body Handles Topical vs. Oral Meds
Topical medications, like diclofenac gel or menthol cream, are meant to stay local. You apply them directly to the skin over the painful joint or muscle. The idea isn’t to flood your whole body with the drug. It’s to get enough into the tissue right where you need it. That’s why most topical NSAIDs have less than 5% bioavailability-meaning only a tiny fraction of the dose actually enters your bloodstream. Oral meds, on the other hand, are built to go systemic. A pill you swallow has to survive your stomach acid, get absorbed through your gut, then pass through your liver before it even reaches your blood. That’s called first-pass metabolism. For some drugs, like morphine, up to 95% of the dose gets broken down before it can do any good. Even for common ones like ibuprofen, you lose about 40% before it ever circulates. This isn’t just science-it’s safety. Less drug in your blood means fewer side effects. That’s why the American College of Rheumatology now says topical NSAIDs should be the first choice for localized joint pain. For older adults especially, skipping the pill avoids stomach bleeds, kidney stress, and high blood pressure spikes.How Much Actually Gets Into Your Blood?
Don’t assume topical means zero absorption. That’s a dangerous myth. If you use a large amount-say, applying gel to both knees, both elbows, and your lower back-you’re not just treating pain. You’re delivering a significant dose systemically. Studies show that with extensive use, topical diclofenac can reach plasma levels of 145 ng/mL. That’s enough to affect your organs. One case report described an elderly patient who developed liver toxicity after using topical NSAIDs daily for months, thinking they were “safe.” The drug didn’t vanish on the skin. It crept in. Transdermal patches are a different story. These aren’t just creams. They’re engineered with chemicals that force drugs through the skin barrier. Fentanyl patches, for example, deliver 92% of the dose into your blood over three days. That’s more efficient than swallowing pills. But that also means they’re powerful-and risky if misused. Topical gels and creams? They’re shallow. Most penetrate only 1 to 3 millimeters into the skin. That’s enough to reach muscles and joint linings, but not enough to reliably treat infections deep inside your body. That’s why antibiotics for pneumonia or UTIs still come as pills. The skin simply won’t let big molecules through.Why Safety Is So Different
Oral NSAIDs are one of the leading causes of hospitalization in people over 65. In the U.S., over 18,000 hospital visits each year are tied to stomach bleeds, kidney damage, or heart problems from these pills. The FDA’s own data shows 14.7 adverse events per 10,000 oral NSAID prescriptions. Topical NSAIDs? Just 1.2 per 10,000. That’s more than 90% lower. Most reactions are mild-itching, redness, or dry skin where you applied it. Contact dermatitis happens in less than 1% of users. No internal bleeding. No kidney strain. No dangerous interactions with blood thinners. The American Geriatrics Society’s 2023 Beers Criteria doesn’t just recommend topical NSAIDs for seniors-it says oral NSAIDs should be avoided whenever possible. Why? Because the risk-benefit ratio flips. For someone with a history of ulcers or heart disease, a topical gel isn’t just safer-it’s life-saving. But here’s the catch: you have to use it right. A 2023 survey of pharmacists found that 41% of topical treatment failures came down to one thing: people didn’t use enough. They dabbed a pea-sized amount on a swollen knee that needed a 4-inch ribbon. Or they applied it once a day instead of three or four times. Skin doesn’t absorb well if you don’t give it enough drug-or enough time.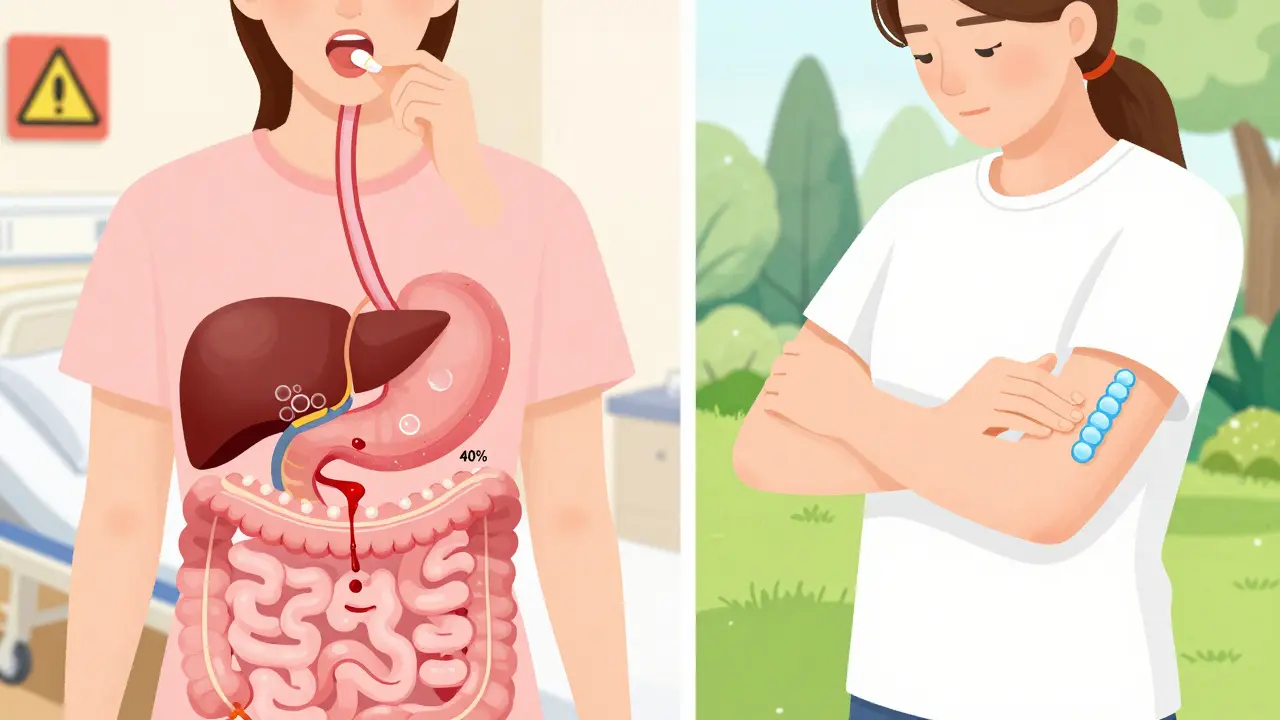
Real People, Real Experiences
In a 2023 survey of over 2,400 people with osteoarthritis, 68% said topical NSAIDs gave them good to excellent pain relief. That’s close to the 72% who said oral meds worked. But here’s the kicker: 89% preferred the topical version. Why? Because they didn’t have to live with acid reflux, bloating, or the fear of a stomach bleed. On Reddit’s chronic pain forums, people regularly write: “No more midnight trips to the bathroom from stomach pain.” Or: “I stopped taking pills after my ER visit for a GI bleed.” But they also complain: “It’s messy.” “It takes too long to work.” “It doesn’t help when it’s cold.” And that’s true. Topical meds absorb slower in cold weather. Skin blood flow drops. The drug sits on the surface longer. If you’re using it for arthritis pain that flares in winter, you might need to warm the area first-maybe a warm towel, or a heating pad on low-before applying.Who Should Use What?
If your pain is in one or two spots-knees, elbows, lower back-topical is your best bet. It’s safer, just as effective for mild to moderate pain, and you won’t be adding stress to your liver or stomach. If your pain is widespread-fibromyalgia, rheumatoid arthritis flares, or post-surgery pain-you’ll likely need oral meds. The skin can’t deliver enough drug to cover your whole body. And if you’re over 65, have kidney issues, take blood thinners, or have a history of ulcers? Skip the pills unless your doctor says otherwise. Topical is the standard of care now.What’s Changing in 2026?
New formulations are coming. Diclonate P, approved in 2023, uses a special gel that pushes diclofenac 3 times deeper into tissue-without raising blood levels. Microneedle patches, currently in late-stage trials, are designed to pierce the top layer of skin with tiny needles and deliver drugs like osteoporosis meds directly into the bloodstream. These could replace pills for conditions that used to require systemic dosing. The market is shifting fast. The global topical drug market grew 7.2% last year-nearly double the growth of oral meds. Insurance companies are catching on too. Medicare now covers 82% of topical NSAID prescriptions, compared to 67% for oral ones. Even though the out-of-pocket cost is slightly higher ($12.40 vs. $9.80), people are choosing them because they avoid hospital visits. Big pharma is pouring money into this. Johnson & Johnson spent $487 million last year on topical delivery tech. Novartis redirected 15% of its NSAID R&D budget away from pills and toward patches and gels.Bottom Line: Choose Smarter, Not Harder
Topical meds aren’t magic. They won’t fix everything. But for localized pain, they’re the smartest, safest option we’ve had in decades. You don’t need to take a pill every day to feel better. You just need to apply the right amount, in the right place, at the right time. Don’t assume topical means no risk. Don’t assume oral is the only way to get relief. And don’t ignore the data: 78% of people who switched from oral to topical NSAIDs stayed on them. Only 22% quit-and most of those said it was because the pain was too severe, not because of side effects. Your body doesn’t need a flood of drugs to feel better. Sometimes, it just needs the right dose in the right spot.Are topical NSAIDs as effective as oral ones?
For localized pain-like osteoarthritis in the knee or elbow-yes. Clinical studies show topical NSAIDs provide pain relief that’s nearly as good as oral versions, with 18% to 92% effectiveness depending on the formulation. But they’re not strong enough for widespread pain, like rheumatoid arthritis flares or post-surgical pain. For those, oral meds are still necessary.
Can topical meds cause side effects?
Yes, but they’re usually mild and local. The most common issue is skin irritation-redness, itching, or dryness at the application site, affecting 10-15% of users. Serious side effects like liver damage or stomach bleeding are rare, but they can happen if you use large amounts over big areas of skin, especially with damaged skin or in older adults. Always follow the recommended dose and avoid applying to open wounds.
Why do some people say topical meds don’t work for them?
The most common reason is improper use. Many people apply too little-sometimes just a pea-sized amount when they need a 4- to 6-inch ribbon. Others don’t apply it often enough; most topical NSAIDs need to be used 3 to 4 times daily. Cold weather also slows absorption. And about 18-22% of people naturally absorb less drug through their skin due to genetics, skin thickness, or circulation issues.
Is it safe to use topical NSAIDs long-term?
For most people, yes-especially compared to long-term oral NSAID use. Studies show topical NSAIDs are much safer for kidneys, stomachs, and the heart. But long-term use still requires monitoring. If you’re using them daily for months, especially over large areas, your doctor should check your liver function and blood pressure. Cases of toxicity have been reported in elderly patients who applied multiple topical products daily without realizing the cumulative effect.
Can I use topical and oral NSAIDs together?
Generally, no. Combining them increases your total NSAID dose without adding much extra pain relief. The risk of side effects goes up, even if the topical one seems “safe.” The FDA and major medical societies advise against combining them unless under direct medical supervision. If one isn’t working, talk to your doctor about switching or adjusting your treatment-not stacking.
What’s better for seniors: topical or oral meds?
Topical NSAIDs are the clear first choice for older adults. The American Geriatrics Society’s Beers Criteria specifically recommends them over oral NSAIDs because they reduce the risk of gastrointestinal bleeding by 82%. Seniors are more vulnerable to kidney damage, stomach ulcers, and drug interactions. Topical delivery avoids most of those risks while still delivering pain relief. Always check with a doctor first, but for localized pain, topical is safer and just as effective.


Comments
beth cordell
I just started using the diclofenac gel after my knee surgery and WOW 🙌 No more stomach chaos. I used to wake up feeling like a warzone in my gut from ibuprofen. Now I just rub it on, watch Netflix, and forget I have arthritis. Also, it smells like a minty forest. Love it. 🌿💊
January 14, 2026 at 01:52
Lauren Warner
Stop romanticizing topical NSAIDs. You're ignoring the fact that 145 ng/mL plasma concentration is still a pharmacologically active dose. This isn't 'safe'-it's just slower poisoning. Elderly patients on multiple meds? They’re getting hit from all sides. The FDA’s own data shows systemic absorption is underreported. This is corporate propaganda dressed as medical advice.
January 14, 2026 at 07:06
Craig Wright
As a British clinician who has treated patients on both sides of the Atlantic, I must emphasize that the data presented here is statistically sound but culturally skewed. In the UK, topical NSAIDs are indeed first-line, but only because oral alternatives are heavily restricted. In the U.S., where pharmaceutical lobbying dictates prescribing norms, this shift is less about science and more about insurance reimbursement incentives. Do not mistake policy for physiology.
January 15, 2026 at 09:34
Lelia Battle
It’s fascinating how we’ve come to equate ‘less systemic’ with ‘safer’ without fully examining what ‘safe’ even means. Is safety the absence of harm, or the presence of sustainable well-being? Topical meds reduce acute risk, yes-but they also reinforce the idea that pain should be suppressed, not understood. What if the real solution isn’t better delivery systems, but better movement, better sleep, better community? The gel gives relief. But does it give healing?
January 15, 2026 at 10:16
Rinky Tandon
Let’s cut through the fluff. Topical NSAIDs are not a panacea. They’re a Band-Aid on a hemorrhage. You’re telling people to slap on gel while ignoring the root causes: obesity, sedentary lifestyles, poor diet, chronic inflammation from processed foods. And now Big Pharma is selling you a placebo with a 7.2% market growth stat. Wake up. The real epidemic isn’t joint pain-it’s medicalization of everyday life.
January 16, 2026 at 10:51
Eileen Reilly
soooo i used the gel for 3 days and it did nothing?? like zero. i applied it like 4x a day and even warmed my knee with a hot towel. my friend said it worked for her. am i just broken?? 😭
January 17, 2026 at 02:00
Monica Puglia
Hey, you’re not broken. Some people just absorb less through their skin-genetics, skin thickness, circulation. Try applying it right after a warm shower, massage it in for a full minute, and give it at least 5 days. Also, make sure you’re using the full recommended amount-not a pea, but a ribbon the length of your finger. You got this 💪
January 17, 2026 at 18:10
Cecelia Alta
Oh please. 68% said it worked? That means 32% said it didn’t. And 89% preferred it? Probably because they didn’t want to admit they wasted $50 on a glorified lotion. I used it for six weeks. My knee still clicked. My doctor told me to stop because I was wasting time. Topical is the new ‘natural remedy’ hustle. If it were truly superior, why do hospitals still give oral NSAIDs to everyone? Because they work. And the gel? It’s just expensive placebo with a fancy label.
January 19, 2026 at 04:29
George Bridges
I’ve been on oral NSAIDs for 12 years. Had two GI bleeds. Switched to topical last year. No more ER visits. No more anxiety about every stomach ache. It takes longer to kick in, sure. But I’d rather wait 20 minutes and feel okay than take a pill and feel like I’m waiting for my body to collapse. This isn’t hype. It’s survival.
January 19, 2026 at 19:30
Faith Wright
Wow. So we’re supposed to be impressed that Big Pharma finally figured out how to sell the same drug without making people vomit? Congrats. You turned a chemical into a lifestyle product. Now we’re all supposed to feel virtuous for choosing the ‘gentler’ option while the real problem-our broken healthcare system-stays untouched. 🙄
January 21, 2026 at 07:42
Rebekah Cobbson
For anyone struggling with the gel: try applying it with a clean finger, then cover the area with a light cotton wrap. It helps with absorption. Also, consistency matters more than intensity. Do it three times a day like brushing your teeth. You’ll be surprised how much better you feel in 10 days. And yes-it’s messy. But so is bleeding ulcers.
January 21, 2026 at 16:01
Audu ikhlas
Topical? In Africa we dont even have access to these fancy gels. We use ginger paste and heat. You Americans think every problem needs a patented solution. This is just capitalism selling you safety like a subscription box. Real pain management is discipline. Not lotion.
January 23, 2026 at 14:58
Sonal Guha
145 ng/mL is still toxic. Stop lying. The data is there. Elderly patients die from this. You think because its on skin its safe? No. Its slower. Its silent. Its worse.
January 23, 2026 at 23:15
TiM Vince
My grandfather used the gel for his hips. He said it felt like a cool breeze on fire. He didn’t talk about it much. Just applied it every night. Didn’t need to. He lived to 92. I think it helped him stay active longer. Sometimes the quietest things are the most powerful.
January 25, 2026 at 18:41
Write a comment