Warfarin-NSAID Bleeding Risk Calculator
Assess Your Bleeding Risk
Your Bleeding Risk
When you’re on warfarin to prevent blood clots, even a simple headache can become dangerous. Taking an over-the-counter NSAID like ibuprofen or naproxen might seem harmless - but it’s not. The combination of warfarin and NSAIDs doesn’t just increase your risk of bleeding. It can send you to the emergency room with a hemoglobin drop of 6 points in less than a day. This isn’t rare. Around 2-3 million Americans take both drugs at the same time, and every year, thousands end up hospitalized because of it.
Why Warfarin and NSAIDs Are a Dangerous Mix
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. Without those factors, your blood takes longer to clot - that’s the point. But NSAIDs work differently. They shut down cyclooxygenase (COX) enzymes, which do two things: reduce inflammation and help platelets stick together to form clots. When you take an NSAID, your platelets can’t do their job properly. So now you’ve got thin blood from warfarin and faulty platelets from the NSAID. It’s a one-two punch that your body can’t handle.
The result? Bleeding happens more often, more severely, and in places you wouldn’t expect. Gastrointestinal bleeding is the most common - think black stools, vomiting blood, or sudden weakness. But intracranial bleeding - bleeding in the brain - is the most deadly. Studies show that combining these drugs raises the risk of brain bleeds by more than 3 times. Even bleeding in the lungs or urinary tract becomes more likely.
Not All NSAIDs Are Created Equal
Many people think if they switch from ibuprofen to celecoxib (a COX-2 inhibitor), they’re safer. They’re wrong. All NSAIDs - whether they’re over-the-counter or prescription - carry this risk. But some are worse than others.
- Naproxen carries the highest risk - 4.1 times more bleeding than warfarin alone.
- Diclofenac is next, at 3.3 times higher risk.
- Ibuprofen is lower, but still dangerous - 1.79 times higher risk.
- Meloxicam and celecoxib are just as risky as traditional NSAIDs when paired with warfarin.
There’s no safe NSAID here. Even low doses, short-term use, or topical forms can still interfere with platelet function. The idea that “just one pill” won’t hurt is a myth. A single dose can tip your INR - your blood’s clotting time - into a dangerous range within days.
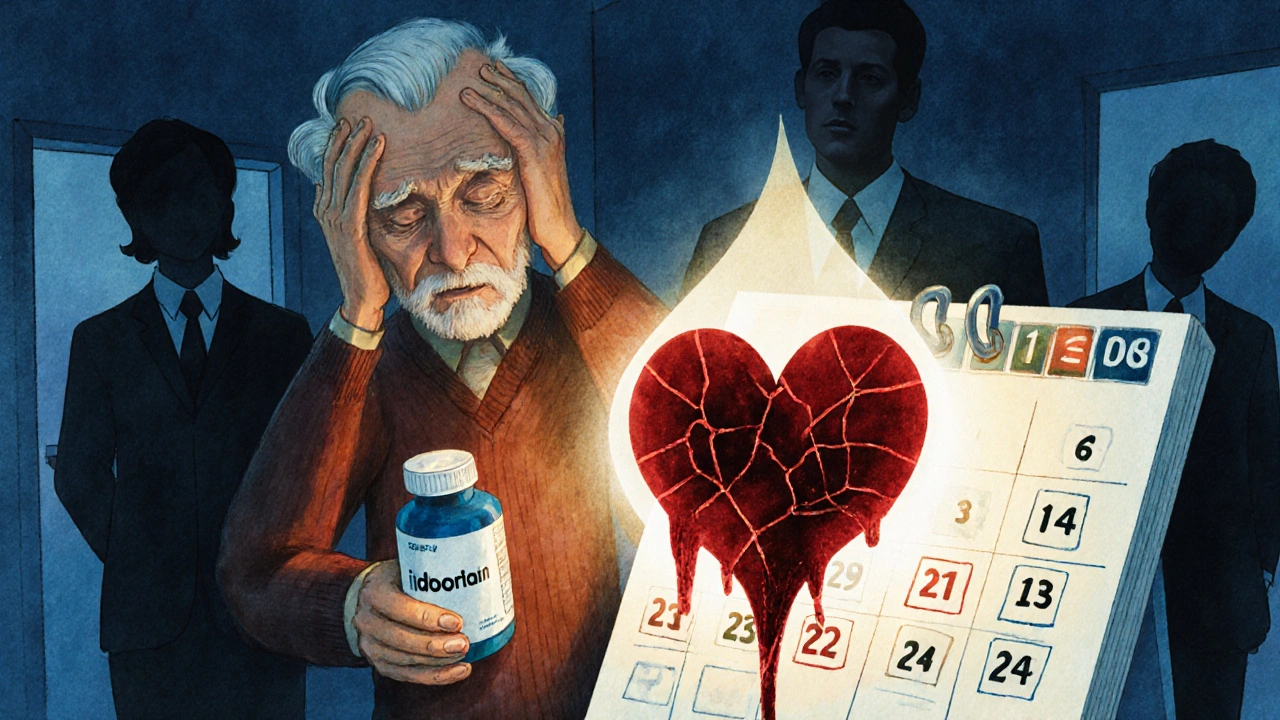
Who’s Most at Risk?
Not everyone on warfarin who takes an NSAID will bleed. But some people are far more vulnerable:
- Older adults - especially those over 75 - have 3.7 times higher risk of bleeding.
- People on high warfarin doses (>40 mg per week) are more likely to see dangerous INR spikes.
- Those taking other medications like antibiotics, antifungals, or SSRIs can have their warfarin levels pushed even higher.
- People with low baseline INR - if your INR was already low before starting an NSAID, adding one can cause a sharp, unpredictable jump.
And here’s the scary part: many of these people don’t even realize they’re at risk. They take ibuprofen for a sore knee, or naproxen for back pain, and assume their doctor knows. But doctors don’t always ask about OTC meds. In fact, studies show that in 68% of bleeding cases, patients didn’t tell their provider they were using NSAIDs.
What About Newer Blood Thinners?
Many patients switch from warfarin to newer anticoagulants like apixaban, rivaroxaban, or dabigatran because they’re easier to manage. But that doesn’t mean they’re safe with NSAIDs.
Research shows that NSAIDs increase bleeding risk with all oral anticoagulants - not just warfarin. The ARISTOTLE trial found that even with apixaban, NSAID use raised bleeding risk significantly. A 2020 study showed dabigatran had slightly lower bleeding risk than warfarin when combined with NSAIDs, but rivaroxaban was just as risky. Bottom line: no oral anticoagulant is safe with NSAIDs.
And here’s the dangerous trend: while warfarin-NSAID co-prescribing has dropped by 27% since 2015, NSAID use with NOACs has risen by 35%. Patients and even some doctors now believe NOACs are “safer” - so they think NSAIDs are okay. That’s a deadly misconception.
What Should You Do Instead?
You don’t have to suffer through pain just because you’re on a blood thinner. There are safer options:
- Acetaminophen (Tylenol) - this is the go-to alternative. It doesn’t affect platelets or INR. Use it at the recommended dose (no more than 3,000 mg/day if you’re on warfarin).
- Topical pain relievers - gels, creams, or patches with lidocaine, diclofenac (topical, not oral), or menthol can help localized pain without systemic effects.
- Physical therapy, heat, or ice - for joint or muscle pain, these non-drug approaches are effective and risk-free.
- Low-dose aspirin - if you’re on warfarin and also need aspirin for heart protection, talk to your doctor. It’s not ideal, but it’s managed differently than NSAIDs.
Don’t assume acetaminophen is always safe either. High doses can affect liver function, which can alter how warfarin is processed. Stick to the label. And never combine it with alcohol.
What If You’ve Already Taken an NSAID?
If you accidentally took an NSAID while on warfarin, don’t panic - but act fast.
- Stop the NSAID immediately.
- Call your anticoagulation clinic or doctor. Don’t wait.
- Get your INR checked within 3 to 5 days - even if you feel fine.
- Watch for signs of bleeding: unusual bruising, nosebleeds that won’t stop, red or black stools, vomiting blood, severe headaches, or sudden weakness.
- If you have any of these symptoms, go to the ER. Don’t wait.
Many patients don’t realize that bleeding can be silent. A slow bleed in the gut can drain your red blood cells over days. You might feel tired, dizzy, or short of breath before you notice anything else. That’s why regular INR checks are non-negotiable when NSAIDs are involved.
How Doctors Should Manage This
Guidelines from the Anticoagulation Forum are clear: if an NSAID is absolutely necessary, follow these steps:
- Use the lowest possible dose for the shortest time - never more than 3-5 days.
- Avoid naproxen, meloxicam, and diclofenac. If you must use one, choose ibuprofen - but still with caution.
- Check INR before starting the NSAID, then again 3-5 days after.
- Consider adding a proton pump inhibitor (like omeprazole) to protect your stomach lining.
- Teach patients to recognize bleeding signs and to report them immediately.
Yet, in practice, this doesn’t happen often. A 2022 report found that 41.7% of U.S. hospitals don’t have electronic alerts in their systems to warn doctors when warfarin and NSAIDs are prescribed together. And most NSAID packaging doesn’t mention warfarin specifically - just generic warnings about bleeding. That’s not enough.

The Real Cost of This Interaction
This isn’t just a medical issue - it’s an economic one. In 2022, bleeding events caused by warfarin-NSAID interactions cost the U.S. healthcare system $1.87 billion. Most of that comes from hospital stays - patients who bleed while on this combo stay in the hospital an average of 5.2 days, compared to 3.8 days for other bleeding causes. Many need blood transfusions. Some need surgery. A few die.
And the human cost? Patient reviews on Drugs.com give this combination a 2.1 out of 10 safety rating. Over 87% of reviews warn others not to do it. One Reddit user wrote: “I took ibuprofen for a headache. My hemoglobin dropped from 14 to 8 in 24 hours. I spent 7 days in the hospital. I’ll never take NSAIDs again.”
What’s Changing?
Things are slowly improving. The FDA added a black box warning to all NSAID labels in 2005. Newer guidelines from the American College of Chest Physicians in 2024 will strengthen the warning against NSAID use with any oral anticoagulant. Researchers are working on NSAID alternatives that don’t affect platelets. AI tools are being tested to flag dangerous combinations before they’re prescribed.
But until then, the message is simple: if you’re on warfarin or any blood thinner, don’t take NSAIDs. Not for headaches. Not for arthritis. Not for back pain. There are safer ways to manage pain - and your life is worth more than a few days of discomfort.
Can I take ibuprofen while on warfarin?
No. Even low-dose ibuprofen increases your risk of bleeding by nearly 80% when taken with warfarin. It can cause your INR to spike unexpectedly, leading to serious bleeding in the gut, brain, or other organs. Acetaminophen is the safer alternative for pain relief.
Is naproxen worse than ibuprofen with warfarin?
Yes. Naproxen carries the highest bleeding risk among NSAIDs when combined with warfarin - about 4.1 times higher than warfarin alone. Diclofenac is next, then ibuprofen. None are safe, but naproxen is the most dangerous choice.
Do COX-2 inhibitors like celecoxib have less risk?
No. Despite early hopes, COX-2 inhibitors like celecoxib and rofecoxib carry the same bleeding risk as traditional NSAIDs when used with warfarin. They still impair platelet function and damage the stomach lining, leading to a doubling of gastrointestinal bleeding risk.
What should I do if I accidentally took an NSAID?
Stop taking the NSAID immediately. Contact your doctor or anticoagulation clinic and get your INR checked within 3-5 days. Watch for signs of bleeding - unusual bruising, black stools, vomiting blood, severe headaches, or dizziness. If you notice any of these, go to the ER right away.
Can I use topical NSAIDs like Voltaren gel while on warfarin?
Topical NSAIDs like diclofenac gel are absorbed in much smaller amounts than oral forms. While the risk is lower, it’s not zero. Some studies suggest a small but real increase in bleeding risk. The safest approach is to avoid them entirely. Use acetaminophen or non-medicated heat/cold therapy instead.
Why do doctors still prescribe NSAIDs to people on warfarin?
Many doctors aren’t aware of the full risk, or assume patients aren’t taking OTC meds. Some think the patient needs pain relief more than they need to avoid bleeding. Others rely on outdated info that COX-2 inhibitors are safe. Electronic alerts in hospitals are often missing or turned off. And patients rarely mention they’re taking ibuprofen for a headache.
Are newer blood thinners like Eliquis safer with NSAIDs?
No. All oral anticoagulants - including apixaban (Eliquis), rivaroxaban (Xarelto), and dabigatran (Pradaxa) - increase bleeding risk when combined with NSAIDs. The risk may be slightly lower with apixaban compared to warfarin, but it’s still significantly elevated. NSAIDs are unsafe with all blood thinners.
Final Takeaway
You don’t need to live in pain just because you’re on a blood thinner. But you do need to be smart about how you manage it. Warfarin and NSAIDs don’t mix - and neither do any other blood thinners and NSAIDs. The data is clear, the risks are real, and the consequences can be fatal. If you’re on warfarin, talk to your doctor about safer pain relief options. And if you’ve ever taken an NSAID without telling your provider, speak up now. Your next INR check could save your life.

Comments
swatantra kumar
Bro this is wild 😱 I took ibuprofen last week for my back pain and thought I was fine... then I felt dizzy and my gums bled for no reason. Now I'm scared to even sneeze. Thanks for the wake-up call 🙏
November 20, 2025 at 16:10
Dave Wooldridge
This is all a government ploy to sell more expensive drugs. NSAIDs are cheap and natural. Warfarin? That's a chemical weapon disguised as medicine. The FDA, Big Pharma, and your doctor are all in on it. They want you dependent. Wake up. The truth is buried under layers of lies and profit motives. 🕵️♂️
November 21, 2025 at 16:50
robert cardy solano
I'm 78 and on warfarin for AFib. Took naproxen for a bad knee last winter. Didn't feel anything until I passed out in the grocery store. Hemoglobin dropped to 7.3. Spent a week in the hospital. No one warned me. Not my cardiologist, not the pharmacist, not even the guy at the drugstore. Just a tiny little warning on the box that no one reads. I'm alive but I'll never trust OTC meds again.
November 22, 2025 at 04:00
serge jane
It's funny how we treat pain like an enemy to be crushed rather than a signal to be understood. We reach for chemicals before we ask why the body is screaming. Warfarin isn't the villain. NSAIDs aren't the demon. It's the assumption that quick fixes are better than slow wisdom. Maybe we should listen more to our bodies instead of our pharmacies. And maybe the real danger isn't the drug interaction-it's the culture that tells us we can't sit with discomfort.
November 23, 2025 at 20:25
Nick Naylor
This is why America is collapsing. You have people taking blood thinners and then popping ibuprofen like candy. No discipline. No responsibility. No understanding of pharmacology. We need mandatory education in high school on anticoagulants. And if you're dumb enough to mix NSAIDs with warfarin, you deserve to bleed out. This isn't a medical issue-it's a cultural failure of basic competence. We're not a nation of patients. We're a nation of idiots with credit cards.
November 24, 2025 at 01:22
Brianna Groleau
I'm from a small town in Louisiana and my grandma used to say 'if it doesn't come from a tree or your kitchen, don't trust it.' She was on warfarin for years and only used heat packs, Epsom salt soaks, and acetaminophen. She lived to 94. I think we've forgotten how to care for ourselves without pills. I shared this post with my whole family. My uncle just stopped taking his naproxen. He's gonna try yoga now. Small changes, big difference. ❤️
November 24, 2025 at 20:45
Rusty Thomas
I took celecoxib for 3 days while on warfarin and thought I was being smart because it was 'COX-2 selective.' Guess what? I woke up with a headache that felt like my skull was splitting open. Turns out I had a tiny subdural bleed. MRI showed it. I was lucky. My doctor said if I'd waited another day I'd have been dead. So yeah, celecoxib is NOT safe. Don't let marketing fool you. I'm now on Tylenol and therapy. My back still hurts but my brain works. 🤕
November 26, 2025 at 12:56
Sarah Swiatek
I'm a nurse who works in anticoagulation. I've seen this exact scenario a hundred times. Patient comes in with INR of 12. No trauma. No fall. Just took ibuprofen for a headache. They always say 'but it was just one pill.' One pill is enough. One pill can kill. We don't even get told when patients are taking OTC meds. Half the time they don't even mention it until they're in the ER. I wish every pharmacy had a pop-up when you buy NSAIDs: 'If you're on warfarin, DO NOT TAKE THIS.' Not a tiny footnote. A neon sign. We're failing people. Every day.
November 27, 2025 at 05:16
Rebecca Cosenza
Don't be reckless. This isn't a suggestion. It's a life-or-death rule. Stop.
November 28, 2025 at 09:50
Pawan Jamwal
In India we have this problem too. People take diclofenac like water. No one checks INR. No one cares. My cousin took it with warfarin and bled internally. Died in 36 hours. His doctor didn't even know he was on blood thinners. We need better awareness. But also, why do Americans have so many drugs? In India, we use turmeric, ginger, massage. Simple. Safe. Why complicate life? 🇮🇳
November 28, 2025 at 19:59
Write a comment