Anticoagulants: What You Need to Know to Stay Safe
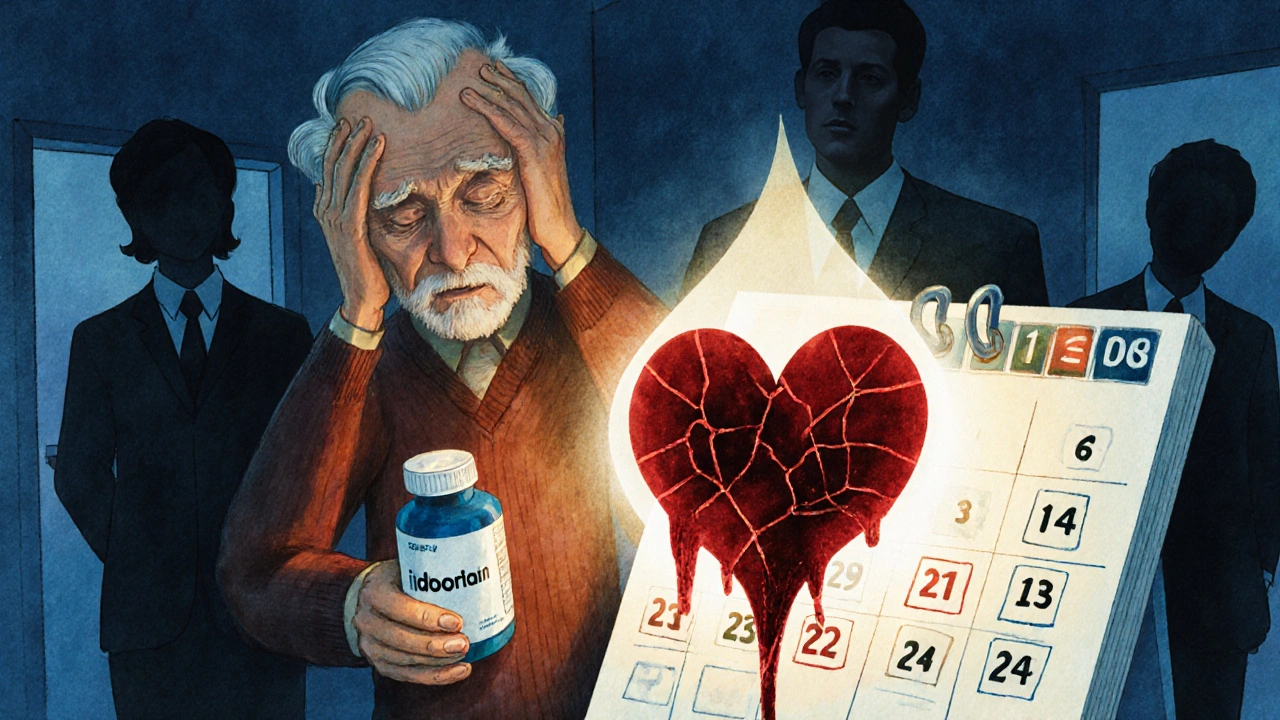
Anticoagulants—often called blood thinners—save lives by preventing clots, but they also raise the chance of bleeding. If you or someone you care for is on one, knowing the basics makes daily life safer and less stressful. This short guide covers what anticoagulants do, the main types, how to reduce risks, and clear signs that need medical attention.
How they work and the main types
Anticoagulants slow your blood’s ability to clot. That’s good when clot prevention is needed—after a stroke, a deep vein thrombosis (DVT), or with some heart conditions. The oldest, warfarin, needs regular blood tests (INR) to keep dosing right. Newer drugs—called DOACs (direct oral anticoagulants) like apixaban, rivaroxaban, dabigatran, and edoxaban—usually need less monitoring and have fewer food interactions.
Heparin and low-molecular-weight heparins (LMWH) such as enoxaparin are often used in hospitals or for short-term treatment. Each drug class has different rules for dosing, missed doses, and reversal if bleeding occurs. For example, vitamin K reverses warfarin; idarucizumab reverses dabigatran; andexanet alfa can reverse certain factor Xa inhibitors.
Practical tips to stay safe every day
Treat anticoagulants like a regular part of your routine. Take your dose at the same time each day and use a pillbox or phone reminder. For warfarin, keep up with INR checks and tell your clinic about any new medicines, supplements, or changes in diet—especially leafy greens, which affect warfarin levels. For DOACs, ask your doctor about kidney function tests; some DOAC doses change with kidney health.
Watch for signs of bleeding: unusual bruises, blood in urine or stool, long nosebleeds, coughing up blood, severe headache, dizziness, or unusual weakness. If you have heavy bleeding or any sudden severe symptom, get emergency care. For minor bleeding or questions, call your prescribing clinician for advice before stopping the drug—stopping suddenly can raise clot risk.
Before any surgery or dental work, tell the clinic you take an anticoagulant. Some procedures require temporary pause or dose change. Carry a card or note listing your anticoagulant, dose, and your clinician’s contact—this helps in emergencies.
Know drug and supplement interactions. Common over-the-counter pain relievers like ibuprofen and aspirin can increase bleeding risk. Herbal supplements such as St. John’s wort, ginkgo, or high-dose fish oil may also interfere with anticoagulant levels. Always check with your clinician or pharmacist before adding new medicines.
Finally, keep regular follow-ups. Labs, kidney checks, or dose reviews help keep therapy safe and effective. If anything feels off—or you plan a new medication, major travel, or pregnancy—reach out to your healthcare team. Anticoagulants work best when you and your clinicians stay connected and alert to changes.
Warfarin and NSAIDs together double the risk of dangerous bleeding. This detailed guide explains why, which NSAIDs are worst, what to use instead, and how to stay safe.
Coumadin (warfarin) is a blood thinner prescribed to prevent clots, and it comes with a lot of rules. This article explains how Coumadin works, why dosing is tricky, what to eat (and avoid), how to stay safe, and the daily realities of living on this medication. It covers everything from INR monitoring to real facts about food and drug interactions, giving you practical advice for dealing with Coumadin in everyday life.