Plasmodium falciparum: Understanding the Deadliest Malaria Parasite
When dealing with Plasmodium falciparum, the parasite that causes the most severe form of malaria in humans, also known as malaria parasite, it’s crucial to grasp how it spreads, how it’s diagnosed, and which medicines work best. Malaria, a disease marked by fever, chills, sweats and anemia arises when infected Anopheles mosquitoes, the night‑biting vectors that transmit the parasite inject sporozoites into the bloodstream. The fight against Plasmodium falciparum hinges on effective antimalarial drugs, medicines such as artemisinin‑based combination therapies (ACTs) and vigilant monitoring of drug resistance, the parasite’s ability to survive standard treatments.
Life Cycle, Symptoms and Diagnosis
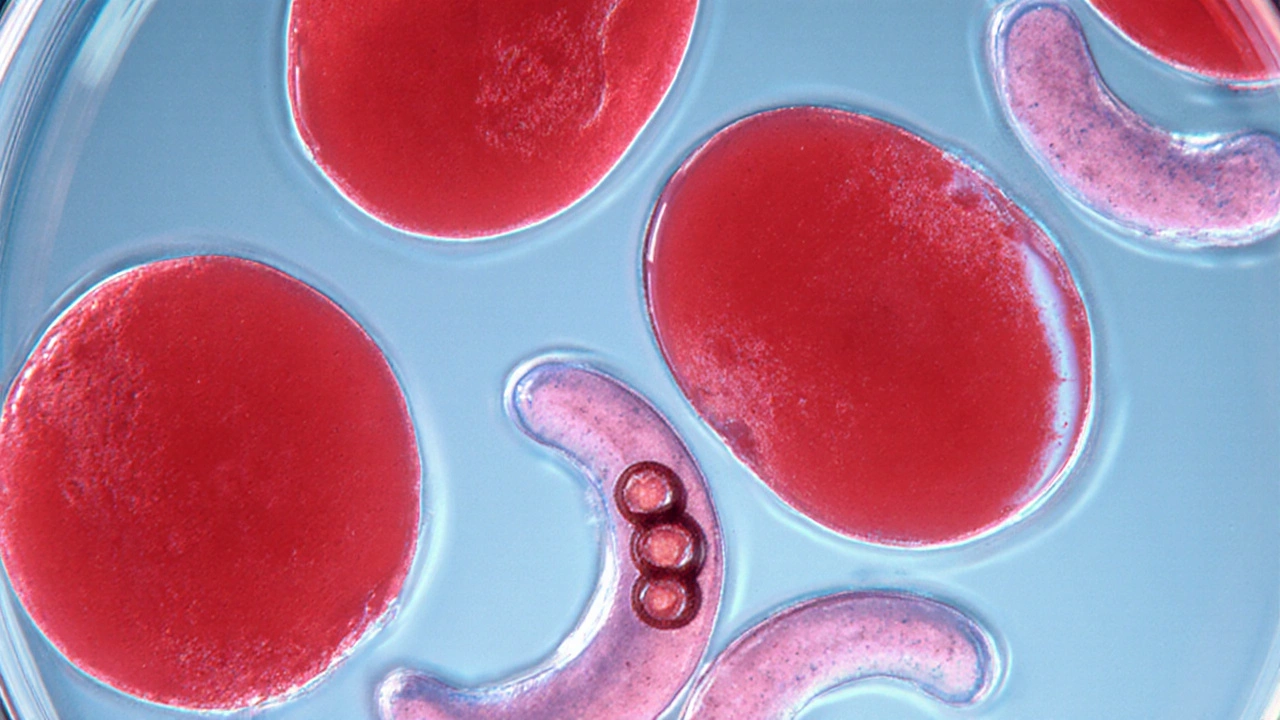
The parasite’s life cycle jumps between the human host and the mosquito. After a bite, sporozoites travel to the liver, multiply, then burst into red blood cells, where they cause the classic fever spikes every 48 hours. Symptoms range from mild flu‑like aches to severe cerebral malaria, which can lead to coma or death. Rapid diagnosis is essential; modern rapid diagnostic tests (RDTs) detect parasite antigens in a finger‑stick blood sample, while microscopy remains the gold standard for quantifying parasite load. Early detection allows clinicians to start treatment before complications develop, saving lives and reducing transmission.
Understanding the link between parasite density and disease severity helps doctors decide whether to hospitalize a patient. High parasitemia (>5% of red cells) often signals a need for intravenous therapy, whereas lower counts may be managed with oral ACTs. In endemic areas, health workers also use clinical algorithms that consider fever patterns, recent travel, and exposure risk. These tools, combined with community education, lower the odds of severe outcomes.
Travelers to malaria‑endemic regions face a unique set of challenges. Pre‑travel consultations should cover prophylactic regimens, insect‑avoidance strategies, and symptom awareness. For short trips, drugs like atovaquone‑proguanil or doxycycline are commonly prescribed, while longer stays may require mefloquine or a more tailored approach based on resistance patterns in the destination country.
Resistance is a moving target. Over the past two decades, resistance to chloroquine and sulfadoxine‑pyrimethamine spread across Africa and Asia, prompting a global shift to ACTs. However, reports of delayed parasite clearance after artemisinin exposure in the Greater Mekong Subregion warn that the parasite can adapt again. Continuous surveillance, molecular testing for K13 mutations, and the development of new drug classes are critical to stay ahead of resistance.
Beyond drugs, vector control remains a cornerstone of malaria reduction. Insecticide‑treated bed nets (ITNs) and indoor residual spraying (IRS) have cut worldwide case numbers dramatically. New tools such as spatial repellents, gene‑drive mosquitoes, and larval habitat management are being trialed to further suppress transmission. Combining these strategies with effective treatment creates a two‑pronged defense: prevent infection and clear parasites quickly when they do appear.
Patients with co‑existing conditions, such as HIV or sickle‑cell disease, may experience altered malaria dynamics. For example, HIV‑positive individuals often have higher parasite densities and may face drug‑interaction challenges with antiretrovirals. Clinicians must adjust dosages and monitor side‑effects closely, ensuring that both infections are managed safely.
Looking ahead, vaccine development offers hope. The RTS,S/AS01 (Mosquirix) vaccine has shown modest efficacy in children, and newer candidates targeting multiple parasite stages aim for higher protection. While a vaccine won’t replace treatment, it could lower the disease burden and buy time for drug pipelines to mature.
In summary, mastering Plasmodium falciparum means understanding its biology, recognizing symptoms early, deploying the right antimalarial drugs, and staying alert to resistance trends. Whether you’re a clinician, traveler, or public‑health worker, the tools listed below will help you navigate the complexities of this parasite and protect yourself and others from its lethal effects.
Explore how sickle cell anemia and malaria are linked through genetics, evolution, and disease outcomes, with clear explanations, data, and practical health tips.